Background
Dry eye disease is no longer limited to geriatric population. In fact, increasing numbers of younger individuals worldwide are affected with DED and India is not an exception. Dry eye disease with its multifactorial etiology impacts not only the vision but also imposes various limitations on the victim. The patient suffers with pain, low vitality and poor general health and experiences poor quality of life (QOL) comparable to medical conditions such as severe angina and those warranting hospital-based hemodialysis. It is important to understand the epidemiology of DED in local population to develop a comprehensive approach that would aid in successful management of this complex disorder.
Aim
To determine novel demographic risk factors that influence DED in the Indian population
Patient Profile
- New patients presenting with DED [recent onset of both symptoms and signs, as defined by the tear film and ocular surface society dry eye work shop (TFOS DEWS) II guidelines] to a multi-tiered ophthalmology network with centers in 200 different geographical locations spread across 4 states of India were included in this study (n=21,290). The patients were enrolled between August 16, 2010 and August 15, 2018.
- Patients with recent onset (≤ 3 months) of occasional, frequent or constant complaints of dryness, grittiness, irritation, foreign body sensation or discomfort; not associated with severe pain, sudden vision loss, itching and discharge, contact lens wear or recent systemic infection were considered positive for DED symptoms.
- Patients with fluorescein break-up time (FBUT) <10s, corneal fluorescein staining of > 5 spots, Schirmer’s test I ≤ 10mm/5 min, abnormal meibomian gland function (poor expressibility, blockage or atrophy) were considered as positive for signs of DED.
- Patients were classified as evaporative, aqueous-deficient or mixed based on the TFOS DEWS II recommendations
Method
Study Design
- Prospective observational hospital-based study conducted across two hundred different locations across four states of India.
Assessments
- Comprehensive ophthalmic examination
Results
- Mean age of the study population was 46.32 years. Of the entire study population 2.11% (n=449) were children and 97.89% (n=20841) were adults.
- The incidence of DED amongst children was 2,688 per million population (0.27%) and that in adults was 16,482 per million population (1.65%) (p<0.0001).
- Overall, the incidence of DED was similar in males and females, but there was an age-decade-wise variation in incidence of DED across male and female genders.
- The incidence of DED was significantly higher in males in 3rd, 4th, 9th and 10th decade (p<0.03) of life. On the contrary, DED incidence was substantially higher among females in 5th and 6th decade (p<0.0001) of life. The incidence of DED did not vary based on gender in the 1st, 2nd, 7th and 8th decade (Table 1).
|
Age Decade |
Odds Ratio (95% CI) |
Gender |
DED Incidence (%) |
P value |
|
0-10 |
1 |
Males |
0.16% |
0.55 |
|
Females |
0.17% |
|||
|
11-20 |
3.7 (0.08) |
Males |
0.63% |
0.234 |
|
Females |
0.61% |
|||
|
21-30 |
10.3 (0.07) |
Males |
2.1% |
<0.00001 |
|
Females |
1.8% |
|||
|
31-40 |
10.2 (0.08) |
Males |
2.2% |
<0.00001 |
|
Females |
1.9% |
|||
|
41-50 |
7.3 (0.08) |
Males |
1.3% |
<0.00001 |
|
Females |
1.7% |
|||
|
51-60 |
8.3 (0.08) |
Males |
1.4% |
<0.00001 |
|
Females |
1.7% |
|||
|
61-70 |
8.4 (0.08) |
Males |
1.4% |
0.088 |
|
Females |
1.5% |
|||
|
71-80 |
10.1 (0.08) |
Males |
1.8% |
0.088 |
|
Females |
1.7% |
|||
|
81-90 |
11.6 (0.1) |
Males |
2.3% |
0.0065 |
|
Females |
1.6% |
|||
|
91-100 |
13.5 (0.23) |
Males |
3.2% |
0.0294 |
|
Females |
1.1% |
- The overall incidence of DED was higher in urban population vs. rural population (59% vs. 41%; p<0.00001).
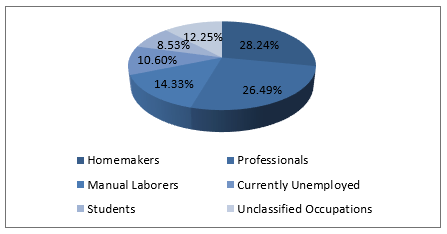
- The incidence of DED was higher amongst homemakers, professionals and people from retired/unemployed category (Figure 1).
- The overall incidence of DED was significantly higher (p<.00001) in the higher socio-economic strata (2.42%; 17,729/731,608) vs. the lower socioeconomic strata (1.19%; 3,561/300,261).
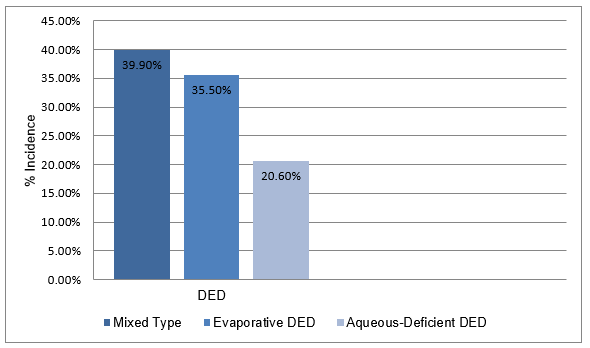
- As per the etiological classification, the prevalence of mixed type of DED was highest, followed by evaporative DED and aqueous-deficient DED (Figure 2).
- As per a multiple logistic regression analysis, increasing age (OR 3.7 to13.5), urban residence (OR 1.6), professional work (OR 1.5); homemaking (OR 1.42), retirement/unemployment (OR 1.24) and socio-economic affluence (OR 1.6 to 3.2) were identified as high risk factors for DED.
- Interestingly, gender predilection varied for different age groups. Thus, males were more likely to develop DED in their twenties and thirties, and females were more predisposed to DED in their forties and fifties.
Conclusions
- Dry eye disease not only impacts the vision but also has an adverse impact on the patient’s quality of life.
- Age, gender, residence (urban/rural), occupation, and socio-economic status have a significant and differential influence on the development of DED. Considering the chronic course of DED, It is believed that an economically developing country like India is on the threshold of a DED epidemic.
- The study reported 1.58% DED incidence rate in the urban population; furthermore, the urban mortality rate as per the latest census data is 0.55%. As the prevalence of DED is expected to rise by 1.03 (1.58-0.55) % annually, it is predicted that nearly 45% of the urban population of India would be suffering with DED by 2030.
- The study reported a DED incidence of 1.31% in rural area. This indicates that 17 million DED patients from rural India will be added every year.
- While comprehensive public health measures are needed to tackle this problem, identification of people at high risk of DED is equally important.
Occul Surf. Feb 22, 2019 (Published Ahead of Print); doi: 10.1016/j.jtos.2019.02.007.

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)