Transurethral Endoscopic Thulium Laser En Bloc Resection of Non-Muscle-Invasive Bladder Cancer Avoids Repeat Transurethral Resection
26 Mar, 20
Introduction
- Standard transurethral resection of bladder tumor (TURBT) – the standard of care in surgery for visible NMIBC lesions, involves piecemeal resection that:
- Does not affect volume of viable tumor cells released during resection
- Causes procedural artefacts in and leaves detrusor muscle (DM) out of resected specimens which leads to pathological understaging, thus leading to underestimation of stage, risk category and sub-optimal treatment
- Eventually, increases risk of tumor recurrence and progression resulting in poor prognosis of the patient
- It often needs to be followed up with a second TURBT which is costly and could cause complications such as bladder perforation
- TmLRBT with its smooth cutting line can yield more complete resection and more accurate diagnosis as it involves en bloc resection with good yield of DM and without artefacts, obviating the need for re-TUR
- Its properties include minimum thermal damage and risk of bladder perforation (due to low penetrability), better hemostasis, and it is also simple to learn
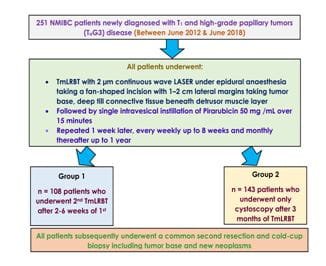
Study Design
Retrospective, single-center, comparative, observational cohort study
Aim
To assess:
- Efficacy of TmLRBT in terms of tumor recurrence and progression
- Whether a single TmLRBT operation can help avoid a second such operation
Methods
Results
- Baseline characteristics were balanced between both groups (p > 0.05 for all features)
- Overall median follow-up time was 40.1 months were: Group 1 – 41.5 months, Group 2 – 39 months (p = 0.32)
- Rate of inclusion of detrusor muscle in all biopsy specimens was 100%
- No patient developed any intra or post-operative complications (Clavien–Dindo classification)
|
Outcomes |
Group 1 |
Group 2 |
p value |
|
Recurrence after common second surgery |
5.6% |
7.7% |
0.52 |
|
Progression after common second surgery |
1.9% |
1.4% |
0.34 |
|
Recurrence during follow-up |
21.3% |
27.3% |
0.34 |
|
Progression during follow-up |
3.8% |
4% |
0.20 |
|
Recurrence-free survival in 1st year |
92.6% |
90.2% |
>0.05 |
|
Progression-free survival in 1st year |
98.1% |
97.9% |
>0.05 |
|
Recurrence-free survival in 3rd year |
84.4% |
80.4% |
>0.05 |
|
Progression-free survival in 3rd year |
96.3% |
95.1% |
>0.05 |
- Recurrence and progression occurred only in patients with T1 tumors and in none with TaG3 tumors
Conclusions
- A single operation of TmLRBT (along with adjuvant intravesical pirarubicin chemotherapy) is cost-effective as it can:
- Prevent recurrence and progression of NMIBC especially in TaG3 tumors
- Obviate the need (as well as costs and complications) of re-TUR by yielding complete resection of visible tumors with almost 100% inclusion of the detrusor muscle layer without any artefacts and no intra- and post-operative complications
BMC Urol. 2020 Mar 18;20(1):30. Doi: 10.1186/s12894-020-00599-1.