Evaluation of the Demographics, Diagnosis and Monitoring, Management, Device Usage and Adherence among COPD Patients: A Survey of Doctors in Malaysia
19 Jul, 18
Introduction
- Globally estimated 384 million people are suffering from Chronic Obstructive Pulmonary Disease (COPD) with a prevalence of 11.7%.1 Current annual mortality is 3 million which might increase to 4.5 million by 2030.1
- With increasing prevalence of smoking in developing countries, and aging populations in high-income countries, the prevalence of COPD is expected to rise over the next 30 years.1
- Translating about 448,000 cases in Malaysia, prevalence of moderate to severe COPD estimated to be 4.7%2
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) recommends the use of spirometer to evaluate the lung function of COPD patients.1
- Guideline also suggests, pharmacologic treatments, and should be complemented by appropriate non-pharmacologic interventions for management of COPD.1
- There is a paucity of recent data to understand the practice pattern of COPD by clinicians in Malaysia.
Aim
- The study aimed to evaluate doctors’ perception on demographics, diagnosis and monitoring, management, device usage and adherence among COPD patients in Malaysia.
Methods
- This was a questionnaire based survey with multiple choices answers.(Figure 1)
- Data was collected from randomly selected 144 doctors of different specialties practicing obstructive airway diseases in both government and private setup.
- The participants were from 10 different locations across Malaysia.
- The data collection took 1 month (November 2017) to complete.
- All forms are hand-filled by the doctors, duly undersigned.
- The data analysis was performed by SPSS version 2.2, supported at Chest Research Foundation (CRF), Pune.
Figure 1: Scheme depicting the execution of the study
Results
- 73% doctors saw at least 5 patients in their daily practice.
- Almost all patients were >40-years of age and more than 90% were smokers.
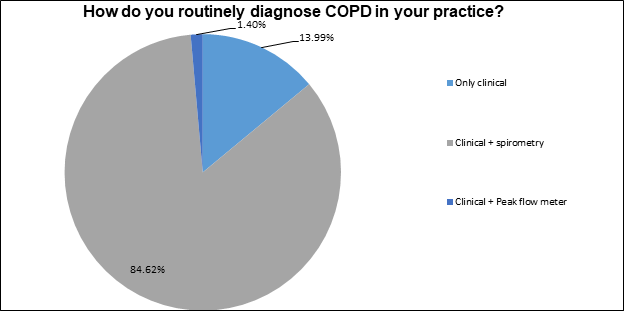
- Most of the doctors routinely used spirometry and clinical judgement to diagnose COPD and suggested a follow-up atleast every 3 months.
Half of the doctors considered patients’ exacerbation history while selecting the treatment for COPD patients.
Figure 2: Response of doctors on method of diagnosing COPD patients
- 85% of doctors routinely use spirometer and clinical examination to diagnose COPD (Fig 2).
- Maximum number of doctors preferred SABA/SAMA combination for Group-A, LABA/LAMA for Group-B and C, and LAMA+ICS/LABA for Group-D patients.
- 64% of doctors prescribed inhalation therapy to all their COPD patients.
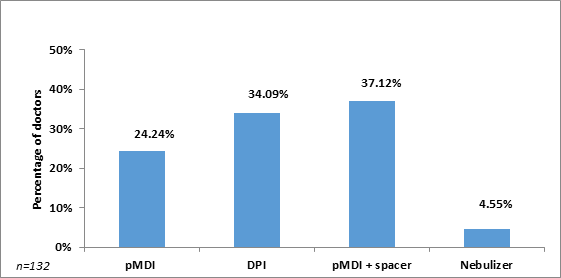
- Pressurised Metered Dose Inhaler (Pmdi) with or without spacer was preferred by most doctors.
- Nebulization in clinic or at home, was one of the preferred options for Group-D patients by 24% of doctors; SABA/SAMA being most prescribed one.
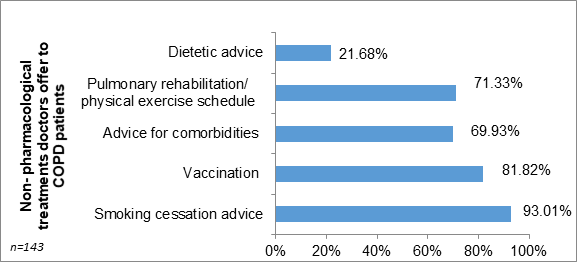
Figure 3: Response of doctors on non-pharmacological treatments offered to COPD patients
- Among the non-pharmacological management, maximum doctors advised for smoking cessation, whereas least being dietetic advice (Fig 3).
Figure 4: Response of doctors on the devices that they prefer to prescribe to maximum number of COPD patients
- pMDI with or without spacer preferred by maximum doctors (Fig. 4).
- 64% of doctors prescribed inhalation therapy to their every COPD patients.
- 13% of doctors believe atleast >70% of their patients are still apprehensive to use inhalers.
- 64% doctors didn’t prefer to prescribe spacer along with inhaler.
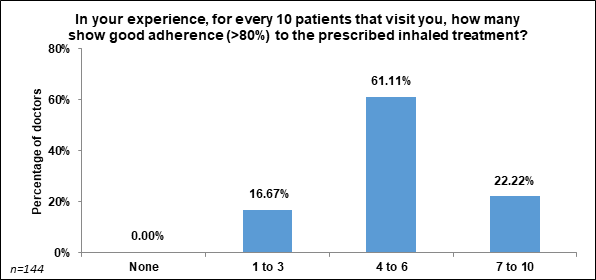
Figure 5: Response of doctors on the number of patients showing good (>80%) adherence to prescribed inhaled treatment, for every 10 patients visited
- Only 22% doctors feel 70% of patients visiting them showed good (>80%) adherence to prescribed inhaled treatment (Fig. 5).
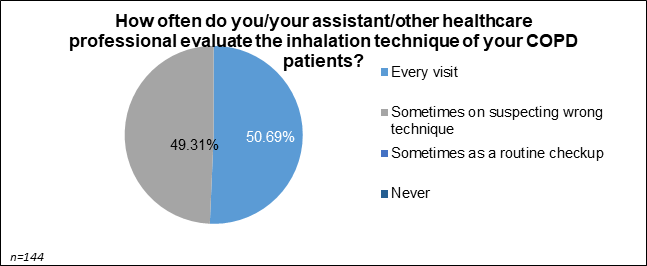
- All the doctors evaluated inhalation technique either at every visit (51%) or on suspecting wrong technique (49%) (Fig. 6).
Figure 6: Response of doctors for the frequency of their evaluation of inhalation technique for patients
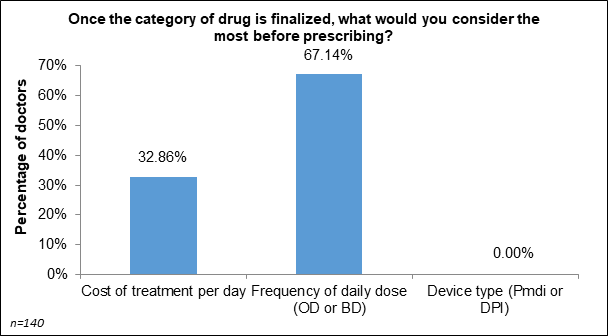
Maximum (67%) doctors considered the number of daily doses most important for their patients, compared to per day cost or type of devices (Fig. 7).
Figure 7 Response of doctor’s consideration for prescription after finalization drug category
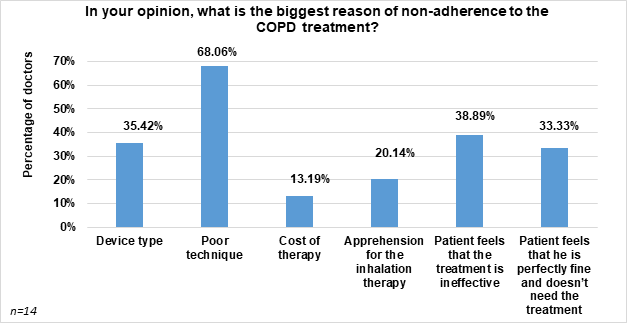
- Poor technique was considered to be the biggest reason for non-adherence to COPD treatment (Fig. 8).
Figure 8: Response of doctor on reason for non-adherence to COPD treatment
Conclusions
- Doctors in Malaysia followed GOLD recommendations for COPD management.
- pMDI with or without spacer is the most preferred device choice for patients with COPD in Malaysia.
- More doctors can adopt inhalation therapy in more number of their patients
- Regular device demonstration in each visit can improve the inhalation technique and possibly can increase adherence to the treatment
References
- Global Initiative for Chronic Obstructive Lung Disease (GOLD) guideline, updated 2018
- Respirology. 2003;8(2):192-198

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)