Effect of Long-term Azithromycin Treatment on Airway Wall Thickness in Patients with SPA
25 Nov, 21
Introduction
Severe persistent asthma (SPA) is a subset of difficult-to-treat asthma that remains uncontrolled despite treatment with high-dose inhaled corticosteroids plus a second controller and (or) systemic corticosteroids, or that worsens when high-dose treatment is decreased.
Aim
To study the effect of long-term treatment with azithromycin on airways wall thickness in patients with severe persistent asthma (SPA)
Patient Profile
Adult (18-65 years) patients with severe persistent asthma
Methods
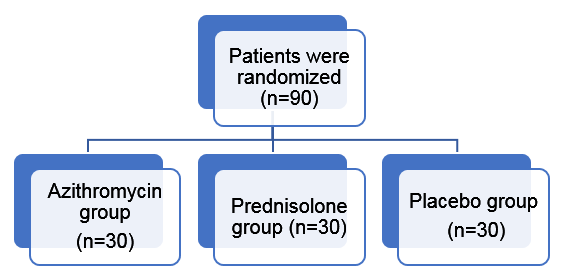
- Randomized, double-blind, placebo-controlled clinical trial
- Study drugs
- Azithromycin (250 mg, BID, three days a week)
- prednisolone (5 mg, BID), or
- placebo for eight months in three separate groups in addition to the standard therapy
Treatment duration: 8 months
Study Outcome
- Primary Outcome: The improvement in right upper lobe apical segmental bronchus (RB1) wall thickness obtained by high resolution computed tomography was set as the primary outcome
- Secondary outcomes: Cough severity, dyspnea severity, asthma control test (ACT) score, asthma exacerbation rate, pulmonary function tests, and fractional exhaled nitric oxide (FENO)
Results
- Bronchial wall thickness percentage did not change significantly in any of the groups
- The inner radius and lumen area of azithromycin and prednisolone-treated subjects increased significantly (p < 0.05 for both)
- Cough, dyspnea severity and Asthma exacerbation rate (AER)
- Azithromycin also significantly improved the dyspnea severity, ACT score, FENO, and FEV1, FEF25-75, and FEV1/FVC (p < 0.05 for all)
- Cough severity or asthma exacerbation rate did not change significantly after eight months of treatment with azithromycin
- The frequency of patients with improved dyspnea severity in the azithromycin group (n = 18) was significantly more than the placebo group (n = 5, p < 0.001)
- Post-treatment AER were 2 [Q1 = 1.5 - Q3 = 3], 2 [Q1 = 1 - Q3 = 2], and 2 [Q1 = 0 - Q3 = 2] for azithromycin, prednisolone, and placebo groups, respectively.
- Median survival days (days without any asthma exacerbation) in azithromycin, prednisolone, and placebo groups were 279, 300, and 205 days, respectively
- ACT score
- Azithromycin and prednisolone groups had a significant increase in the ACT scores (p < 0.001 for both).
- The mean change of ACT score from baseline in the azithromycin group (3.52 ± 2) was significantly less than the prednisolone group (6.2 ± 2.2) but significantly more than the placebo (0.7 ± 2.4) group (p < 0.001 for both)
- FENO
- Post-treatment FENO was 23 [Q1 = 11 - Q3 = 83.5], 22 [Q1 = 7 - Q3 = 80], and 28.5 [Q1 = 19 - Q3 = 42.25] in azithromycin, prednisolone, and placebo groups, respectively
- FENO in azithromycin and prednisolone groups reduced significantly (p < 0.05 for both)
- Lung function
- FEV1, FEV1/FVC, and FEF25-75 increased significantly in both azithromycin and prednisolone groups (p < 0.05 for all)
- Safety
- No significant difference in the frequency of adverse events, serious adverse events, or adverse events leading to discontinuation of the study drug were observed (p > 0.05 for all)
Conclusion
- Long-term treatment with azithromycin demonstrated increased lumen radius and lumen area in patients with severe persistent asthma
- The study highlighted the ability of azithromycin in improving clinical findings, including dyspnea severity, ACT score, and pulmonary function tests
- The data suggest that azithromycin is a potentially useful add-on treatment option in patients with SPA, but it has no effect on airway wall thickness
Reference
Respiratory Medicine.2021;185:106494
Related Topics