Prevalence of Methicillin-Resistant S. aureus Infection among Patients in the Emergency Department
Introduction
Methicillin-resistant staphylococcus aureus (MRSA) has emerged as a cause of infection among patients exposed to the bacteria in health care settings. Recently, MRSA infections have been reported among persons in the community without established risk factors for MRSA. When compared to health care associated(HA) MRSA isolates, community associated(CA) MRSA tend to be resistant to a few antibiotics, produce different toxins and have a different kind of a gene complex known as staphylococcal cassette chromosome mec (SCCmec) which contains the mecA gene that confers methicillin resistance. However, limited data is available regarding the prevalence as well as the association of MRSA as a cause of skin and soft tissue infections among the patients from different communities in US.
Aim
To determine the prevalence of MRSA as a cause of skin infections among adult patients presenting to emergency departments in several geographically diverse, metropolitan areas in the United States.
Patient Profile
- N= 422
- Patients with skin and soft-tissue infections
- Median age 39 years
- Race or ethnic group
- 49 percent of patients were non-Hispanic blacks
- 25 percent were non-Hispanic whites
- 22 percent were Hispanic
- 4 percent belonged to other groups
- Infections were classified as an abscess in 81 percent of patients, an infected wound in 11 percent, and as cellulitis with purulent exudate in 8 percent
Methods
Study Design
- Prospective prevalence study
- Conducted in hospitals in the EMERGEncy ID Net, a network of university-affiliated emergency departments in 11 U.S. cities
Results
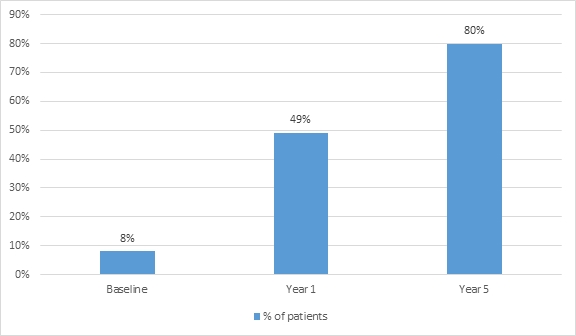
- S. aureus was isolated from 76% (320 of 422) patients with skin and soft-tissue infections.
- Out of the S.aureus isolated from 320 patients, 78% (249 patients) were MRSA
- The overall MRSA prevalence was 59 percent and ranged from 15 % to 74%
- On genetic and phenotypic characterization, 97 %of MRSA were found to be pulsed-field type USA300. 74% of these were a single strain (USA300-0114).
- SCCmec type IV and the Panton–Valentine leukocidin (pvl) toxin gene were detected in 98 percent of MRSA isolates
- MRSA susceptibilities were as follows
- 95 percent to clindamycin
- 6 percent to erythromycin
- 60 percent to fluoroquinolones
- 100 percent to rifampin and trimethoprim–sulfamethoxazole
- 92 percent to tetracycline
- Antibiotic therapy was not concordant with the results of susceptibility testing in 100 of 175 patients with MRSA infection who received antibiotics (57 percent)
- Among methicillin-susceptible S. aureus isolates, 31 percent were USA300 and 42 percent contained pvl genes
Conclusion
MRSA was the most common pathogen isolated in the emergency department from patients with skin and soft-tissue infections. Strategies used for patients with confirmed MRSA infections should be considered for all patients with purulent skin and soft-tissue infections in areas with a high prevalence of MRSA.
N Engl J Med 2006; 355:666-74.