Introduction
The decision to hospitalize patients with community-acquired pneumonia (CAP) and antimicrobial choice have been recommended to be based on validated scoring systems, such as CURB-65. In spite of this, documentation of severity scores for unscheduled admissions has been poor. Sometimes, the patients having low CURB-65 score are unnecessarily admitted and the use of antimicrobials is not in accordance with the guidelines. The admitted patients are poorly managed leading to high hospital length of stay (LOS) and prolonged use of antibiotics.
Aim
This audit evaluated whether antimicrobial stewardship of in-hospital CAP could be improved with an intervention bundle.
Methods
Study Design
- Comparison of retrospective data (Aug-Sep 2018) to post-intervention prospective data (May-June 2019)
Treatment Strategy
- A retrospective cohort of hospitalized CAP patients were compared to a postintervention prospective cohort
- The intervention bundle comprised of a mobile audience response system, promotion of the antimicrobial app, development of a physical card with local guidelines, and incorporating CURB-65 into the unscheduled admission proforma
- Local guidelines were in line with the British Thoracic Society CAP guidelines Patients with CAP were identified from Hospital In-Patient Enquiry data
- Patients with consolidation on chest radiography admitted to emergency department were recruited
- Compliance with antimicrobial guidelines was defined as correct route, dose and frequency
- If additional antibiotics were given despite otherwise complete adherence the episode was considered non-adherence.
Endpoints
- Compliance with antimicrobial guidelines
- LOS
- Mortality
- Duration of intravenous and total antibiotics
- Documentation of CURB-65 score
- Uptake of appropriate investigations
Results
- The study population comprised of a total of 69 adult patients aged >18 years; 37 pre-intervention (retrospective) and 32 post-intervention (prospective)
- The mean ± S.D. CURB-65 score was 2.16 ± 1.17, and 50 patients (72.5%) had a CURB-65 score of ≥2
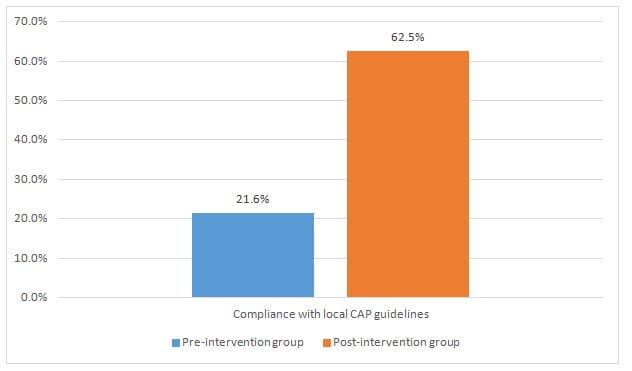
- Most of the patients (92%) received intravenous antibiotics. The most common antibiotic used was amoxicillin/clavulanic acid (n = 41; 59.4%) while clarithromycin was the second most common (n = 34; 49.3%).The post-intervention group had a significantly higher compliance with antimicrobial local CAP guidelines (p<0.001) as shown in Figure 1.
- Although the duration of initial intravenous antibiotic duration was similar in both groups, a difference was seen in total antibiotic duration preintervention versus post-intervention as shown in Table 1.
|
|
Pre-intervention group |
Post-intervention group |
P value |
|
Duration of IV antibiotics (days) |
4 (2-4.5) |
4 (2-5) |
0.70 |
|
Duration of total antibiotics (days) |
9 (7-11) |
7 (6.5-9) |
0.01 |
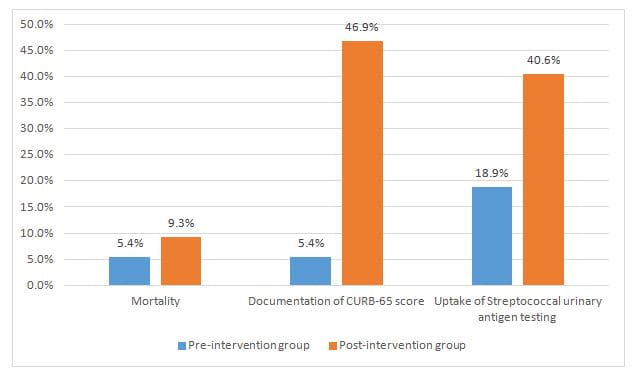
- Mortality rate was similar in both groups as shown in Figure 2.
- However, the prospective cohort had better documentation of CURB-65 (p<0.001) and better uptake of streptococcal urinary antigen testing (p=0.024) as shown in Figure 2.
Conclusion
- A simple, low-cost quality intervention bundle can significantly increase appropriate antimicrobial prescribing, appropriate investigations and reduce the duration of the total antibiotics.
J Glob Antimicrob Resist. 2020 Dec; 23:38-45.