Introduction
Terbinafine and itraconazole are commonly used oral antifungals for dermatophytic infections. Widespread resistance to conventional doses of antifungals with increasing clinical failure rates warrants the search for an effective first?line antifungal drug that brings about rapid clinical and mycological cure in tinea corporis and tinea cruris
Aim
To compare the efficacy of oral terbinafine versus itraconazole in the treatment of tinea corporis and tinea cruris
Patient Profile
Patients of both genders aged 18 years and above with clinical diagnosis of tinea corporis and tinea cruris confirmed by potassium hydroxide (KOH) test
Methods
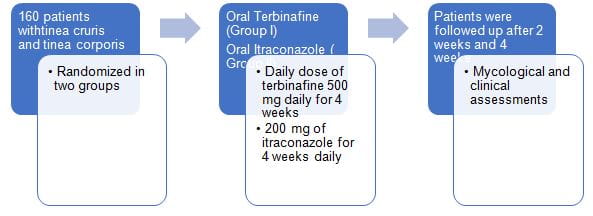
- Randomized comparative study
Assessments
- At each visit, clinical response was noted, including pruritus, erythema, and scaling. These were rated as clinical score 0–3, 0 – absent, 1 – mild, 2 – moderate, and 3 – severe
- Global clinical evaluation was done, and the response was noted accordingly as healed, marked improvement, considerable residual lesions (>50%), no change, or worse
- Monitoring of signs and symptoms for any adverse cardiac event was done at each visit
- Patients were considered cured when there was an absence of scaling, erythema, and pruritus, and KOH was also negative
Results
|
Parameters |
Group 1 Terbinafine (n=160) |
Group 2 Itraconazole (n=160) |
|
Age (mean±SD) |
34.97±14.123 |
34.78±13.039 |
|
Gender, n (%) |
|
|
|
Male |
103 (32.3) |
107 (33.5) |
|
Female |
56 (17.6) |
53 (16.6) |
|
Diagnosis |
|
|
|
Tinea cruris |
11 (3.4) |
7 (2.2) |
|
Tinea corporis |
10 (3.1) |
5 (1.6) |
|
Tinea cruris et corporis |
129 (40.3) |
135 (42.2) |
|
Tinea cruris et corporis with faciei |
10 (3.1) |
13 (4.1) |
No statistically significant difference in the above parameters. SD=Standard
deviation
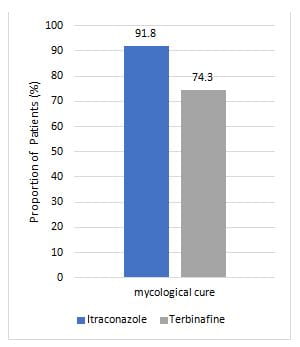
- The global clinical response at the end of 4 weeks was significantly better in the itraconazole group as compared to the terbinafine group.
- More patients in Group II were in the healed category as compared to Group I (46% vs 37%).
- Only a few patients worsened in the itraconazole group (Group I) as compared to the terbinafine group (Group II) (4.1% vs 12.2%)
- At the end of 4 weeks, there was a statistically significant improvement in erythema, scaling, and pruritus scores in Group I as well as in Group II
|
Parameters |
Mean±SD (%) |
P values between groups | |
|
Group 1 (n=160) |
Group 2 (n=160) | ||
|
Pruritus |
|
|
|
|
Baseline to 2 weeks |
21.7±30.4 |
19.8±24.8 |
0.637 |
|
2 weeks to 4 weeks |
24.0±31.3 |
31.3±23.3* |
0.028 |
|
Baseline to 4 weeks |
45.6±44.5*,# |
51.0±29.4*,# |
0.861 |
|
Scaling |
|
|
|
|
Baseline to 2 weeks |
5.4±23.3 |
−4.8±21.4 |
<0.001 |
|
2 weeks to 4 weeks |
16.7±28.0* |
29.6±19.1* |
<0.001 |
|
Baseline to 4 weeks |
22.1±35.0*,# |
24.8±21.2*,# |
0.698 |
|
Erythema |
|
|
|
|
Baseline to 2 weeks |
15.4±31.0 |
17.3±27.5 |
0.449 |
|
2 weeks to 4 weeks |
16.9±22.7 |
15.6±18.3 |
0.386 |
|
Baseline to 4 weeks |
32.3±38.6*,# |
32.9±25.9*,# |
0.372 |
Within?group comparison *P<0.05 as compared to the baseline to 2 weeks, #P<0.05 as compared to 2?4 weeks. SD=Standard deviation
- Tolerability and compliance to the drug were similar in both the groups
- Mild adverse effects such as gastrointestinal upset, headache, and taste disturbances were observed which were comparable in both the groups
Conclusions
- Itraconazole demonstrated higher clinical and mycological cure rates as compared to terbinafine.
- Itraconazole seems to be superior to terbinafine in the treatment of tinea corporis and tinea cruris
Reference
Indian J Pharmacol 2019;51:116-9.