Introduction
- Urethral obstruction (most commonly due to BPH) is a common condition among elderly males
- Elderly patients who have often failed medical therapy are frequently ineligible for major surgery (which requires general anesthesia) for a variety of reasons (≥ 1 of):
- Advanced age and associated complications
- Post-cerebrovascular disease (cognitive, sensory and motor deficits)
- Anticoagulant therapy, which could be risky to interrupt
- Detrusor underactivity (Decompensated hypocontractile bladder)
- The standard or most common alternative required to manage such cases – transurethral insertion of a Foley catheter, is however associated with complications (such as trauma) and challenges of long-term management:
- They have to be changed monthly and hence require monthly visits by patient (and caregivers)
- Thus, cause psychological stress and interfere with daily activities of both patients and their families
- Temporary (easily removable) prostate stent presents a convenient and effective alternative. Being a one-time procedure, it can also decrease load on the healthcare system and medical costs
- However, there are no data on its long-term efficacy and safety
Study Design
Prospective, single-center, pre-post, non-randomized interventional study
Aim
To assess:
- Long-term efficacy and safety of TEmt
- Whether TEmt facilitates removal of Foley catheter in such patients
- Patient clinical factors associated with greater efficacy and safety
Methods
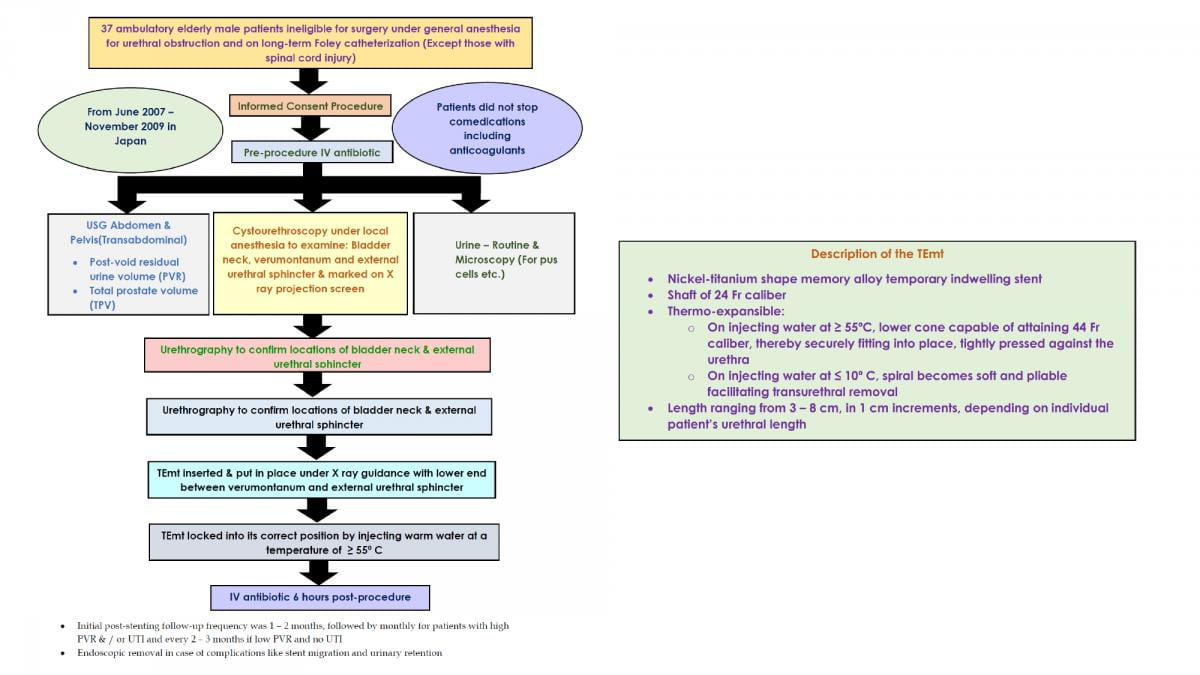
Study Flow Diagram & Description of the Intervention
Results
- Baseline characteristics of patients are mentioned in table 1 (n = 37 patients)
|
Baseline characteristic |
Mean ± SD (Range) or Number (%) |
|
Age (In years) |
79.8 ± 6.2 (66 – 91) |
|
ECOG Performance status (PS) (Higher the worst) | |
|
PS: 0 |
16 (43%) |
|
PS: 1 |
5 (14%) |
|
PS: 2 |
13 (35%) |
|
PS: 3 |
2 (5%) |
|
PS: 4 |
1 (3%) |
|
Total Prostate Volume (mL) |
50.2 ± 31.6 (6.1 – 122) |
|
Duration of Foley Catheter Insertion (months) |
14.1 ± 16.8 (1 – 78) |
|
Cerebrovascular disorders |
11 (29.7%) |
|
Anticoagulant therapy |
14 (37.8%) |
- A positive correlation (linear relationship) was found between prostatic urethral length (PUL) and total prostate volume (TPV)
- The stent lengths used ranged from 3 cm – 7 cm with 4 cm being most common
- Mean post-stenting follow-up duration was 33.2 months (SD = 16.7 months)
- Post-stenting improvements in outcomes are given in table 2
|
Outcomes |
Post-stenting improvement - % / Mean ± SD (Range) |
|
Unassisted voiding a day after stenting |
100% |
|
Unassisted voiding 3 months after stenting |
57.1% |
|
Post-void residual urine volume (PVR) <50 cc |
76.4% |
|
Post-void residual urine volume (PVR) (cc) |
42.7 ± 66 (0 – 288) |
|
Improvement in pyuria (≥ 50 pus cells / high power field) |
52% |
|
Improvement in activities of daily living & quality of life |
100% |
|
High treatment satisfaction |
100% |
- Removal of Foley catheter occurred in 100% patients with unassisted voiding
- Unassisted voiding was difficult in patients with poor PS as compared to those having good PS (p = 0.04)
- ~19% patients had stent migration, of whom ~71% had a TPV < 20 cc. Thus, a small prostate size (TPV < 20 cc) appears to be a risk factor for stent migration
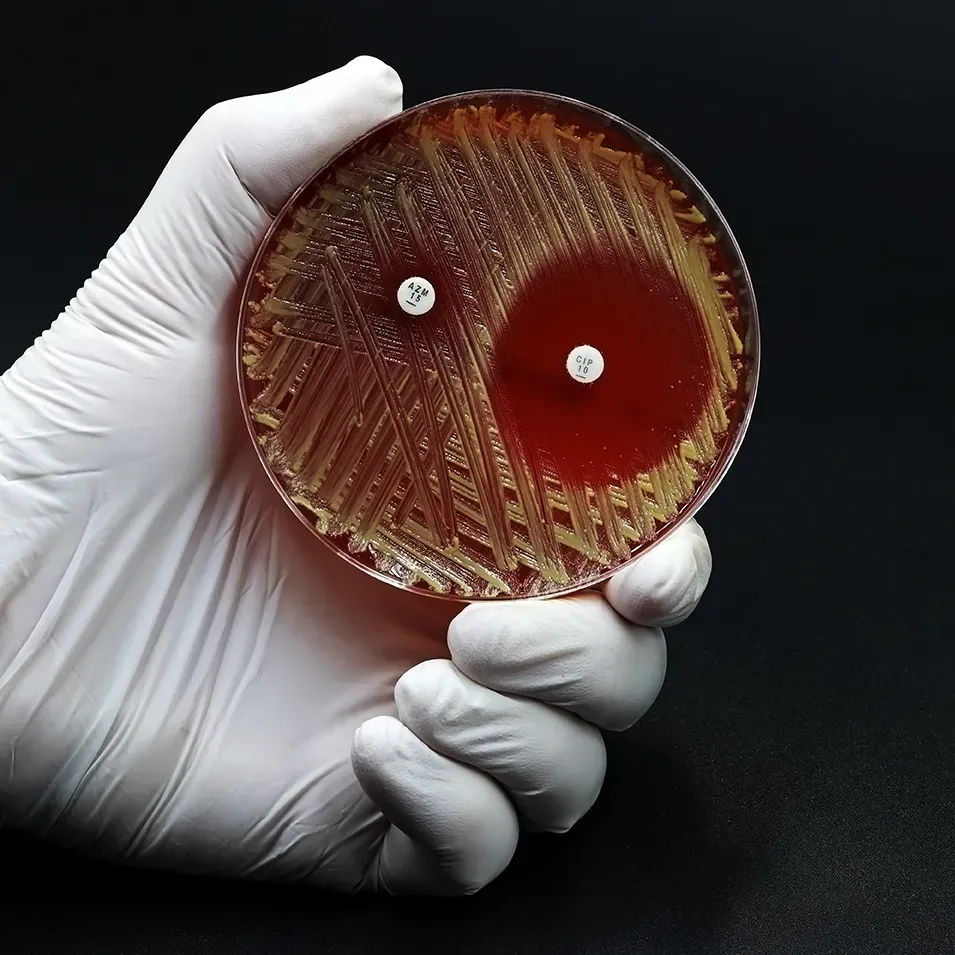
- No serious adverse effects such as hematuria, urinary retention, thrombosis, calculus or calcification were seen though some patients did get UTI (one of whom had sepsis)
Conclusions
- TEmt stents are effective and safe in elderly male patients with urethral obstruction who are ineligible for major surgery and require long term Foley catheterization
- They facilitate removal of Foley catheter, can be effectively used over the long term and are especially suited for patients with good PS and higher TPV
Geriatr Gerontol Int. 2015 May;15(5):553-8. Doi:10.1111/ggi.12309.