Preserve the Precious: Diabetes, a Silent Invader
What is Diabetic Retinopathy?
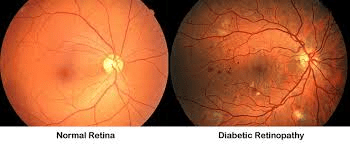
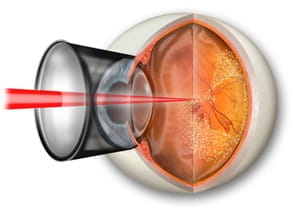
Diabetic retinopathy (DR) is a condition that occurs in people who have diabetes. It causes progressive damage to the retina, the light-sensitive lining at the back of the eye. Diabetic retinopathy is a serious sight-threatening complication of diabetes.
Diabetes interferes with the body’s ability to use and store sugar (glucose). The disease is characterized by too much sugar in the blood, which can cause damage throughout the body including the eyes.
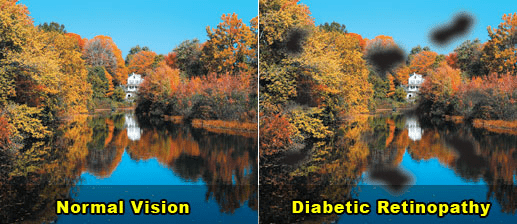
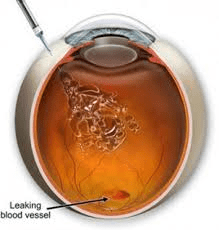
Over time, diabetes damages the blood vessels in the retina. Diabetic retinopathy occurs when these tiny blood vessels leak blood and other fluids. This causes the retinal tissue to swell, resulting in cloudy or blurred vision. The condition usually affects both eyes. The longer a person has diabetes, the more likely they will develop diabetic retinopathy. If left untreated, diabetic retinopathy can cause blindness.
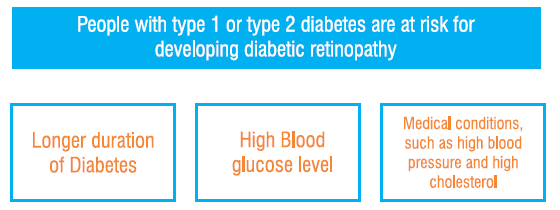
Who is at risk for developing DR?
What are the symptoms of DR?
Seeing spots or floaters
Blurred vision
Difficulty seeing well in night
Seeing blank or dark areas in your field of vision
How can diabetes hurt the retina of my eyes?
- Retina damage happens slowly
- Retinas have tiny blood vessels that are easy to damage
- First, these tiny blood vessels swell and weaken. Some blood vessels then become clogged and do not let enough blood through
- At first, you might not have any loss of sight from these changes
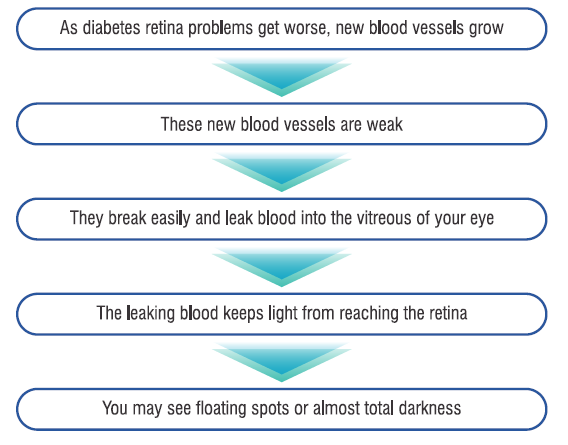
What happens as diabetes retina problems get worse?
What are the four stages of diabetic retinopathy?
Mild Non-Proliferative Retinopathy
The features of mild non-proliferative retinopathy are some of the earlier stages of diabetic retinopathy. At this point, small areas of balloon-like dilation of blood vessels, called microaneurysms, start to appear along with other findings such as small spot hemorrhages and cotton wool spots. It's important to note that not all patients with mild non-proliferative retinopathy will notice a change in their vision.
Moderate Non-Proliferative Retinopathy
Moderate non-proliferative retinopathy is essentially a progression from the mild stage. Many more microaneurysms, hemorrhages and cotton wool spots emerge and there is further damage to the retinal blood vessels. The danger is that such damage can result in reduced blood flow to the surrounding retinal tissue leading to vision loss.
Severe Nonproliferative Retinopathy
As the retinopathy progresses and more blood vessels have now been affected, larger areas of the retina are deprived of blood flow. This results in the retina producing new blood vessels in an attempt to enhance nourishment.
Proliferative diabetic retinopathy (PDR)
At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels that grow along the retina and into other parts of the eye. These blood vessels are abnormal and fragile, often leading to the development of new or worsening existing symptoms and frequent vision loss. Left untreated, severe vision loss and even permanent blindness can result.
How is Diabetic Retinopathy detected?
Dilated Eye Exam
During this exam, dilating eye drops are put in the eyes to make the pupils dilate (open widely) to allow a better view of the inside of the eye, especially the retinal tissue. Regular dilated eye exams by an ophthalmologist are important, especially for those who are at a higher risk for diabetic retinopathy or diabetes.
Optical Coherence Tomography
Provides highly detailed cross-sectional images of the retina that show its thickness, helping determine whether fluid has leaked into retinal tissue.
Fluorescein Angiography
A retinal photography test called fluorescein angiography (FA) is done to evaluate the retina blood vessel circulation. After dilating the pupils, a dye is injected into the patient’s arm. The dye then circulates through the eyes and works like a food coloring. As the dye circulates, the ophthalmologist takes pictures of the retina to accurately detect blood vessels that are closed, damaged, or leaking fluid. The pictures are black and white to help the doctor detect these changes more easily.
With proper examinations, diabetic retinopathy can be detected before vision loss begins.
How will my Diabetic Retinopathy be treated?
DR can be treated with several therapies that may be used alone or in combination.
Anti-VEGF Injection Therapy
Anti-VEGF drugs are injected into the vitreous gel to block a protein called vascular endothelial growth factor (VEGF), which can stimulate abnormal blood vessels to grow and leak fluid. Blocking VEGF can reverse abnormal blood vessel growth and decrease fluid in the retina. Available anti-VEGF drugs include bevacizumab, ranibizumab and aflibercept.
Most people require monthly anti-VEGF injections for the first six months of treatment. Thereafter injections are needed less often: typically, three to four during the second six months of treatment, about four during the second year of treatment, two in the third year, one on the fourth year, and none in the fifth year.
Laser surgery
In laser surgery, a few to hundreds of small laser burns are made to leaking blood vessels in areas of edema near the center of the macula. Laser burns slow the leakage of fluid, reducing swelling in the retina. The procedure is usually completed in one session, but some people may need more than one treatment.
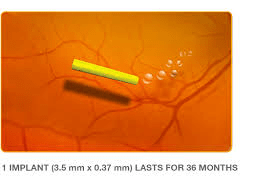
Corticosteroids
Corticosteroids, either injected or implanted into the eye, may be used alone or in combination with other drugs or laser surgery to treat DME.
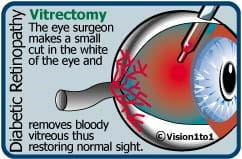
Vitrectomy
A vitrectomy is the surgical removal of the vitreous gel in the center of the eye. The procedure is used to treat severe bleeding into the vitreous, and is performed under local or general anesthesia. During the surgery, vitreous gel filled with blood is removed and replaced with salt solution and with silicone oil in case of retinal detachment. Vitrectomy may be performed as an outpatient procedure or as an inpatient procedure, usually requiring a single overnight stay in the hospital. After treatment, the eye may be covered with a patch for days to weeks and may be red and sore. Drops may be applied to the eye to reduce inflammation and the risk of infection. If both eyes require vitrectomy, the second eye usually will be treated after the first eye has recovered.
Will I go blind if I suffer from Diabetic Retinopathy?
Yes. If the disease progresses & is not treated, there is a chance of vision loss.
What can I do if I have already lost some vision from Diabetic Retinopathy?
If you have lost some sight from diabetic retinopathy, ask your doctor about low vision services and devices that may help you make the most of your remaining vision.
What Can I do to protect my vision?
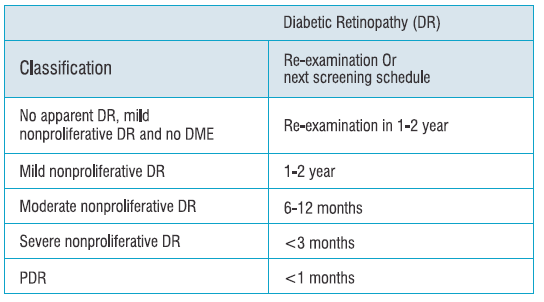
Vision lost to diabetic retinopathy is irreversible. However, early detection and treatment can reduce the risk of blindness by 95 percent. Because diabetic retinopathy often lacks early symptoms, people with diabetes should get a comprehensive dilated eye exam at least once a year. People with diabetic retinopathy may need eye exams more frequently and should adhere to their follow-up schedules.
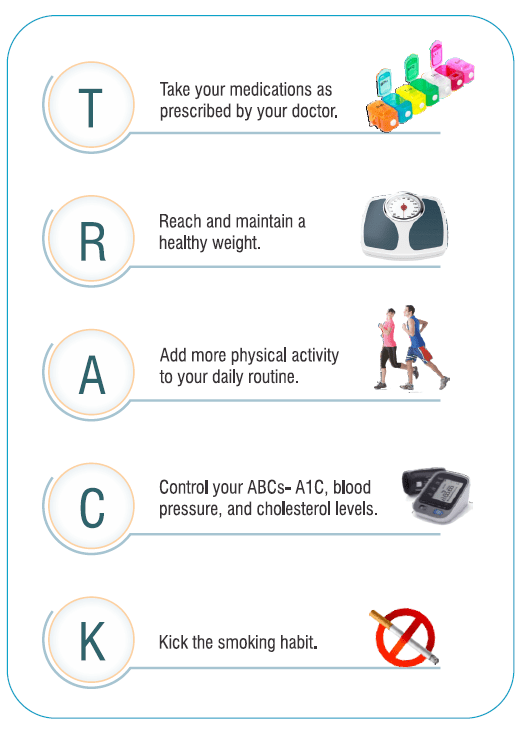
If you have diabetes, it’s important to keep your health on TRACK
References
- http://rgw.com/patient-education/eye-diseases/diabetic-retinopathy. Last accessed on 02/04/2019.
- ICO Guidelines for Diabetic Eye Care (Updated 2017)
- www.london-eye-surgeon.co.uk. Last accessed on 02/04/2019.
- https://www.aoa.org/patients-and-public/eye-and-vision-problems/glossary-of-eye-and-vision-conditions/diabetic-retinopathy. Last accessed on 02/04/2019.