Air Pollution: Should We Care About the Air We Breathe?
Air Pollution: Why should we Worry?
Air pollution is becoming a major risk factor for health problems and affects millions of people worldwide. Environmental exposure to air pollutants increases the rates of cardiovascular and respiratory morbidity and mortality.
Fast Fact: Humans need to inhale around 10,000 litres of air every day to provide the body with vital oxygen required for survival and health. The quality of air we breathe therefore determines not only the health of the lungs, but also of other organs in the body.
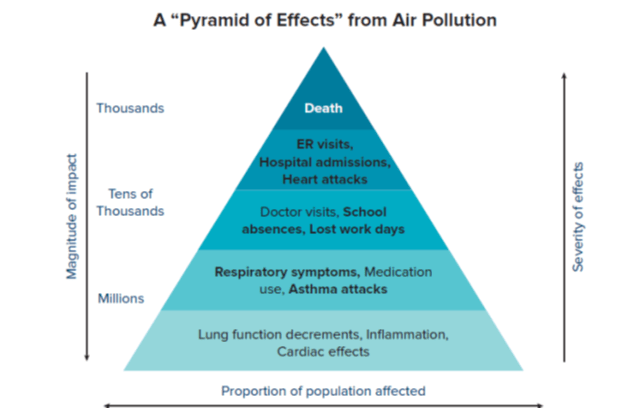
Figure 1 depicts the magnitude of impact air pollution has on our health.
Fast Fact: Air pollution was responsible for 8 million deaths globally in 2012 as per the WHO reports. 3.7 million deaths attributable to ambient air pollution. 4.3 million deaths attributable to household air pollution.
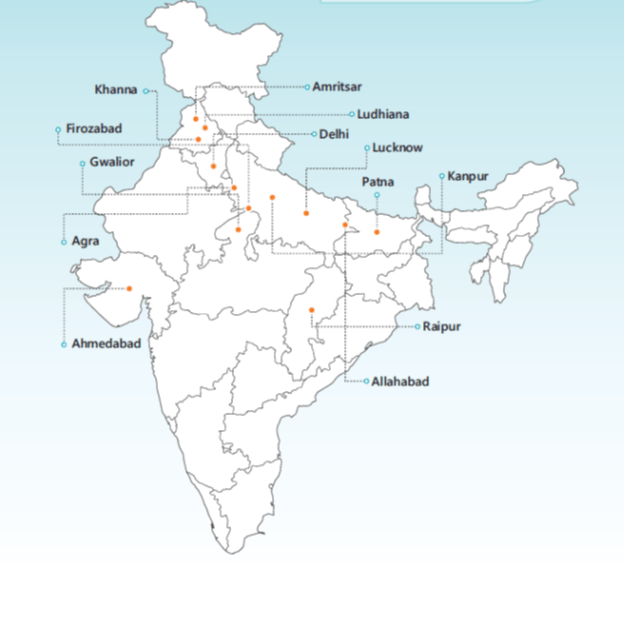
Recently, the World Health Organization reported that 13 of the 20 most polluted cities in the world are in India! These include cities as shown below.
Respiratory System is the Prime Target!
Inhalation of the air pollutants into the respiratory tract, makes it the prime
target for harmful effects (Figure 2).
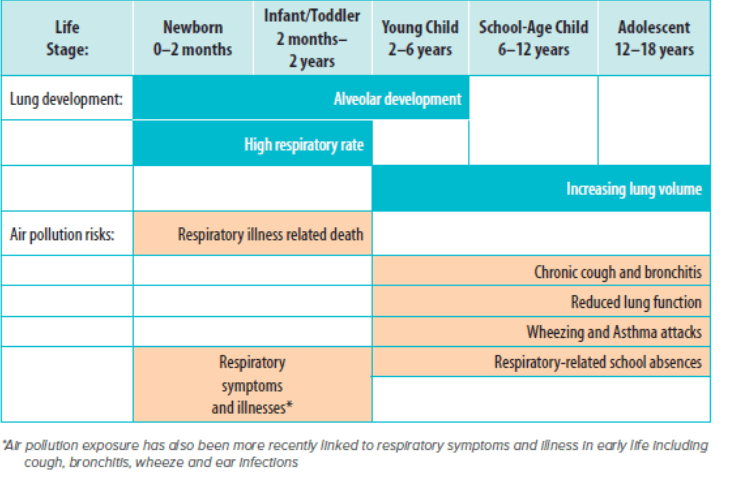
- Although exposure to air pollution effects all age groups, there is emerging evidence that exposure during pregnancy and early childhood increases the risk of adverse health outcomes.
- Exposure during early pregnancy may interfere with the placental development and delivery of oxygen and nutrients to the foetus. In infants and young children, it can easily alter lung development and lung function as the child’s lungs are vulnerable in this growing phase.
- Delhi tops the list of cities with worst air quality. A study examining the effects of air pollution in Delhi on respiratory symptoms and associated morbidity, was conducted by Central Pollution Board in 2008. The findings suggested that Delhi had 1.7 times higher prevalence of respiratory symptoms (in past 3 months) compared with rural controls in West Bengal (P<0.001), the odds ratio of upper respiratory symptoms being 1.59 and 1.67 for lower respiratory symptoms.
Effects of Air Pollution on Respiratory System & Vulnerable Population
Fast Fact: Diesel exhaust particles have been shown to increase the allergenicity of allergens by around 50 times.
- People with genetic predisposition to atopy tend to develop a Th2 mediated airway inflammation along with increased IgE production when exposed to air pollutants. Acute inflammatory responses and exacerbations are more likely to develop.
- Pollutants can cause lung damage due to oxidative stress by acting directly on the production of free reactive oxygen species (ROS), inducing epithelial cell inflammation, airway hyperactivity and lung injury. They reduce the levels of antioxidants in the lungs and therefore make it more vulnerable to the harmful effects of air pollution.
- Air pollutants can damage airways and can also cause inheritable changes in the gene expression due to non-coding changes in the DNA (termed as epigenetics) leading to the development of asthma.
Fast Fact: Exposure to high levels of air pollutants can induce changes in DNA, which means the damaging effects can be transmitted to the next two generations, making them more vulnerable to the effects of air pollutants.
- Several molecular mechanisms (genetics and epigenetics) have been suggested linking air pollution and its effects on the lungs and the airways –
- The effect of air pollutants on lung health is dependent on various factors like the size and composition of particles, the level and duration of exposure, age and also the sensitivity of the individual.
- The common air pollutants affecting the respiratory system are Particulate Matter (PM), Nitrogen dioxide (NO2), Sulphur dioxide (SO2), Carbon Monoxide (CO) and Ozone (O3).
The table below (Table 1) shows the common air pollutants, their deposition in the respiratory tract and possible pathophysiology & effects.
|
Air Pollutants |
Deposition |
Effects |
|
Particulate Matter (PM, PM2.5, PM10) |
Trachea, bronchi, bronchioles, alveoli, lung tissue and bloodstream
|
|
|
Nitrogen dioxide (NO2)
|
Trachea, bronchi, bronchioles and alveoli
|
|
|
Sulphur dioxide (SO2) |
Upper airways, trachea, bronchi and bronchioles
|
|
|
Carbon Monoxide (CO)
|
Alveoli and bloodstream
|
|
|
Ozone (O3)
|
Trachea, bronchi, bronchioles and alveoli
|
|
Young children, pregnant women, patients with pre-existing disease, elderly, etc, who experience elevated risks from the exposure of the pollutant are considered vulnerable groups (Table 2).
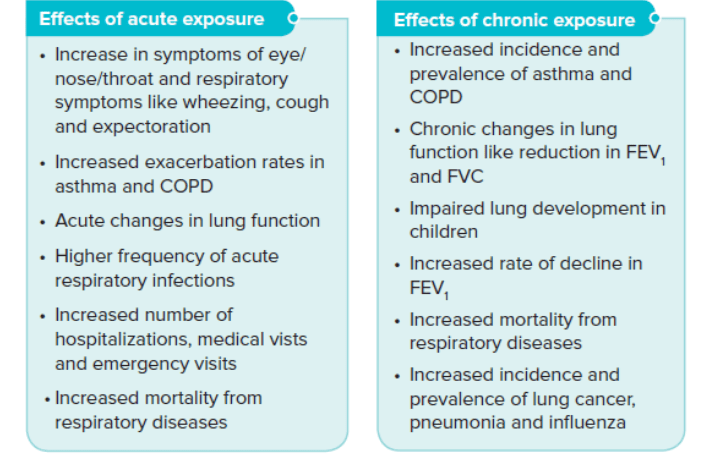
The deleterious effects of air pollution are also dependent on the level of pollutant exposure, i.e. short-term exposure or acute exposure (hours, days, or weeks) and long-term exposure or chronic exposure (months or years), (refer Table 3).
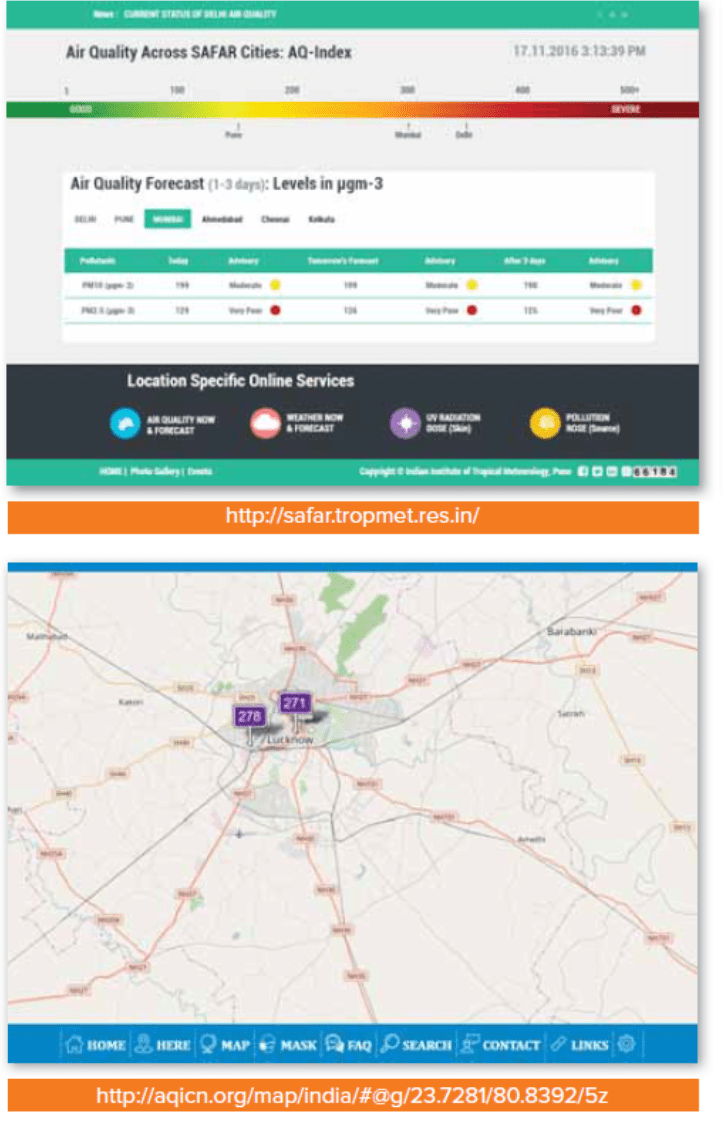
Measuring Air Pollution Levels
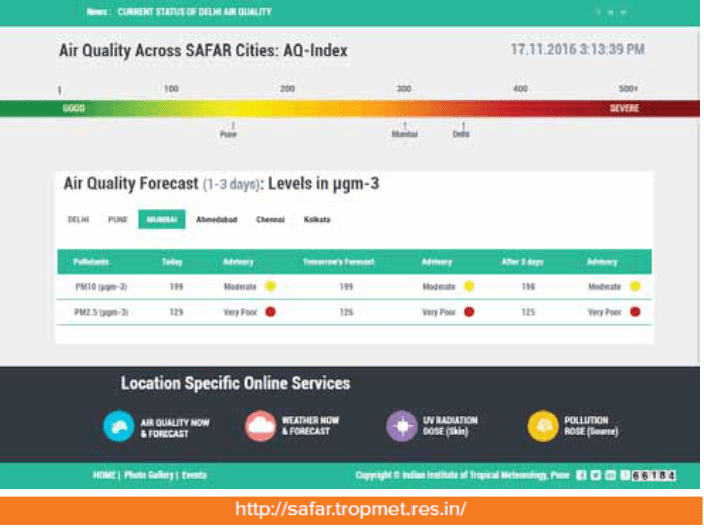
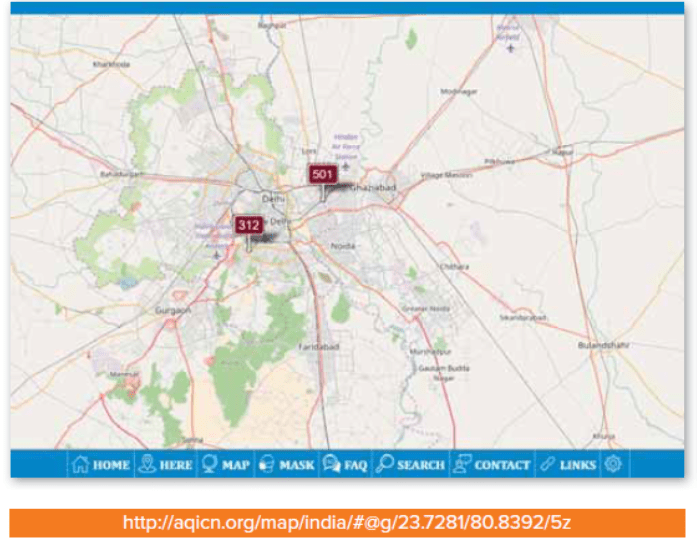
- Measuring air pollution levels can provide information to healthcare professionals, patients and even healthy individuals about the air quality around the area. A key tool to measure pollution levels is Air Quality Index (AQI) which reports air quality on daily basis.
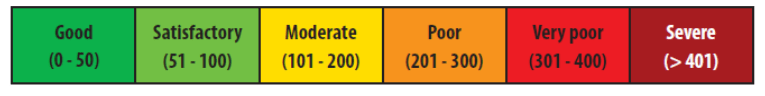
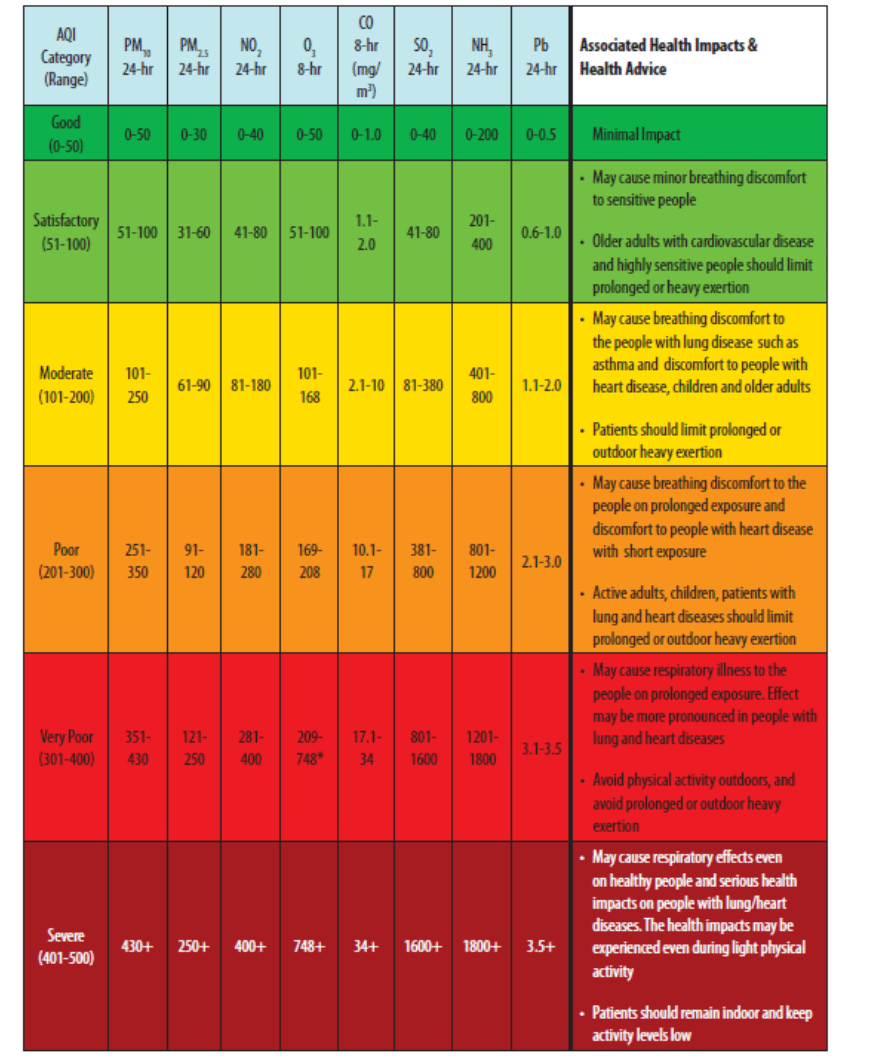
- The AQI in India has been categorized as good, satisfactory, moderate, poor, very poor and severe and is colour coded. The colour coding can help nearby residents to decide the necessary precautions to be taken.
Reading the AQI is simple and is also easily accessible through internet. The AQI reading starts with 0 and runs till 500, which is the highest.
- The table below (table 4) presents the AQI breakpoints measured in microgram (or milligram in the case of CO) per cubic meter for eight air pollutants including, PM, SO2, NO2, O3, CO, along with its health impact.
- Higher the AQI value, higher is the level of air pollution and greater health concern. AQI less than 100 is good and satisfactory, however, AQI more than 300 is poor and can be hazardous.
- If AQI levels are above 100, the air quality is considered to be unhealthy especially for certain sensitive groups of people.
In most situations, it is difficult to avoid exposure to air pollution, hence reducing the risk is an important step, by knowing the AQI levels and avoiding outdoor activities when it is very high.
The AQI levels can be accessed online at
- http://safar.tropmet.res.in/
- http://aqicn.org/map/india/#@g/22.0888/80.6085/5z
It is also available on android and apple app stores.
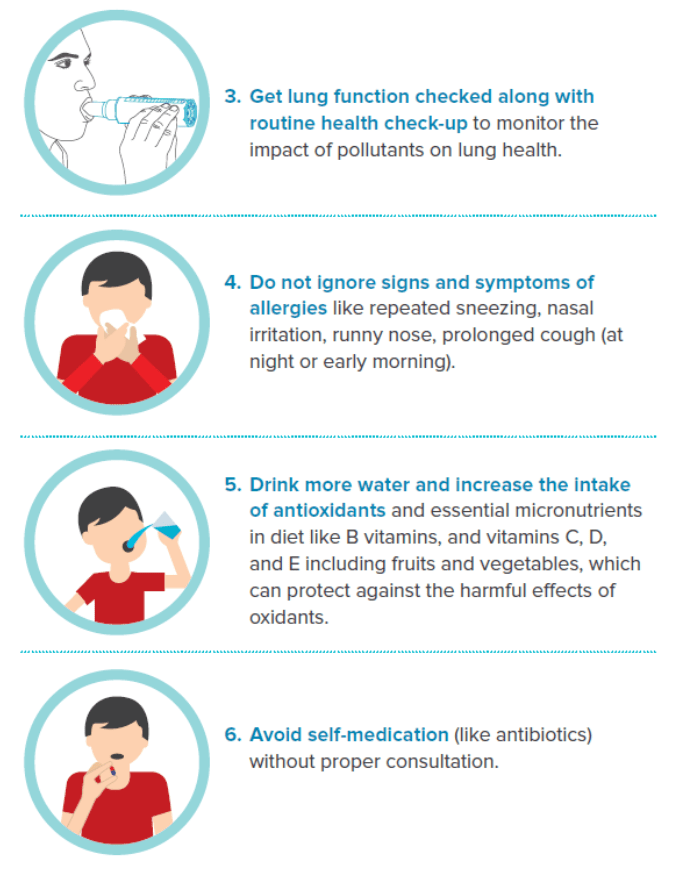
Essential Steps to Protect against the Potentially Harmful Effects of Pollutants
In Healthy Individuals
1. Pay attention to the AQI levels: Avoid/plan outdoor activities according to the AQI levels. Examples as shown below:
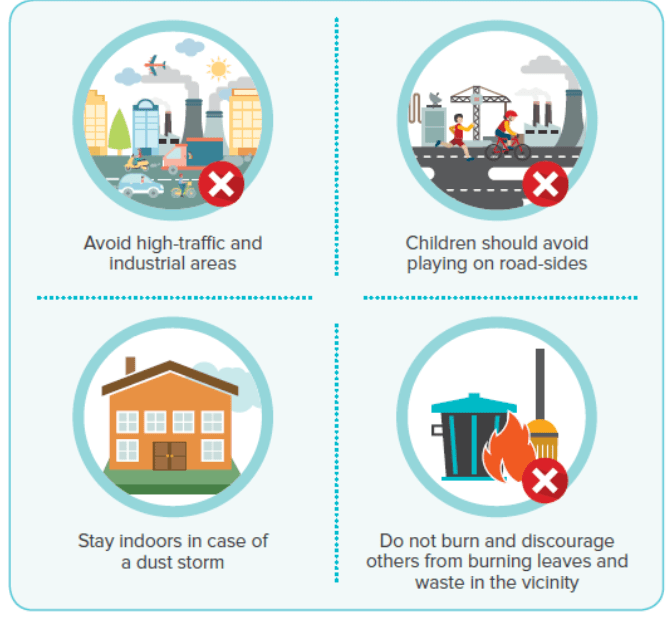
2. Minimize exposure to pollutants
Reduce exposure to outdoor air pollutants
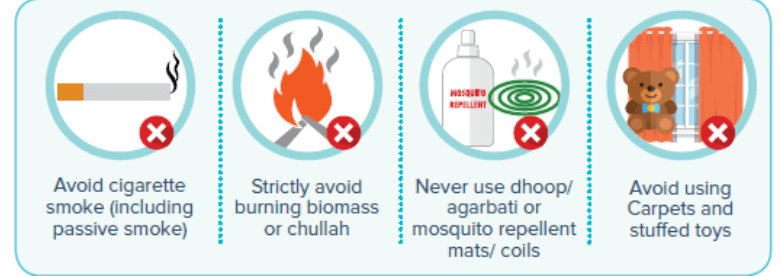
Avoid exposure to indoor pollutants
Since, it may be difficult to avoid all the triggers; the sources of pollutants can be reduced and people should be educated and counselled by the clinicians.
In Patients with Existing Disease (e.g. asthma and COPD)
1. Pay attention to the AQI levels: Avoid/plan outdoor activities according to the AQI levels. Examples as shown below:
2. Minimize or limit prolonged exposure to pollutants, as these may exacerbate symptoms
Reduce exposure to outdoor air pollutants
Avoid exposure to indoor pollutants like
- Avoid dry brooming of floor. Prefer wet mopping / vacuum cleaning.
- Bedding should be given a hot water wash once in 3-4 days.
- Use dust mite resistant covers for mattress and pillow. Otherwise keep them in the sun for about 4 hours once in 10 days.
- Do not use perfumes / deodarants / talc / room-freshners.
- Avoid using chalk as far as possible.
- Prevent seepage / dampness / cockroach buildup in the home.
- Avoid exposure to kitchen fumes.
- Avoid keeping a pet. If you have a pet, groom it daily and keep out of sleep area.
- Proper ventilation of indoor spaces is also important.
- Fumes generated by fresh paint and wood polish to be avoided as far as possible.
- Avoid keeping indoor plants.
- Take adequate precautions against viral infections by following general hygienic practices and vaccines where required/ advised.
Since, it may be difficult to avoid all the triggers; the sources of pollutants can be reduced and people should be educated and counselled by the clinicians.
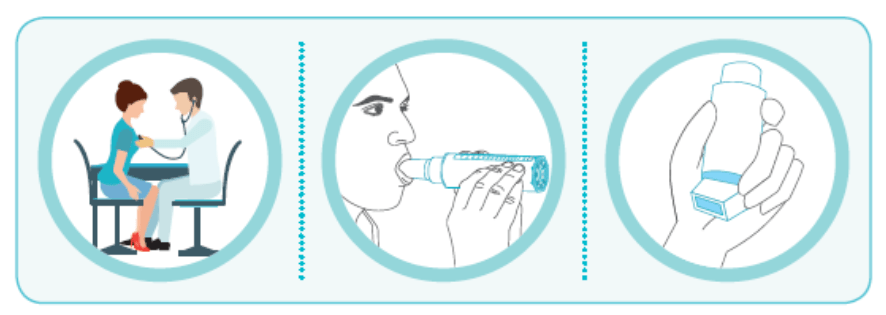
3. Regular reviews/check-ups of the existing disease with the healthcare provider can be helpful.
4. Self-monitoring with peak flow meter: Monitoring lung function regularly can help in adjusting the medication dose, as per the action plan provided by the healthcare provider, especially in asthmatics.
5. Regular use of controllers like inhaled corticosteroids inhaled corticosteroids + long acting ?2-agonists / anti-leukotrienes, in asthmatics and nasal inhaled corticosteroids, anti-histamines for allergic rhinitis, can help in controlling the symptoms and reducing the risk of exacerbation, which may occur due to uncontrolled disease.
6. Patients should always carry reliever inhaler (SOS medication) like salbutamol / levosalbutamol / levosalbutamol + ipratropium, whenever prescribed.
7. N-acetylcysteine can be beneficial in reducing the oxidative stress, especially in patients with COPD.
8. Healthy diet with high antioxidants and essential micronutrients (such as B vitamins, and vitamins C, D, and E) including fruits and vegetables to be included, which can protect against the harmful effects of oxidants.
9. Avoid self-medication (like antibiotics) without proper consultation.
10. Do not contribute to environmental air pollution:
- Reduce dependence on personal vehicles. Use public transport and carpools, etc. as far as possible.
- Plant more trees.
- Use air-conditioners sparingly and operate them at 25° or above.
References
1. http://www.who.int/topics/air_pollution/en/ (accessed on 6th Jan, 2016)
2. http://www.epa.gov/benmap/how-benmap-ce-estimates-health-and-economic-effects-air-pollution (accessed on 6th Jan, 2016)
3. http://www.environment.ucla.edu/reportcard/article1700.html (accessed on 6th Jan 2016)
4. TherAdv Chronic Dis 2015, Vol. 6(5) 286– 298
5. Nutrients 2015; 7: 10398–10416
6. Can Fam Physician 2011;57:881-7
7. J Thorac Dis 2015;7(1):23-33
8. https://www.asthma.org.uk/advice/triggers/pollution/ (accessed on 8th Jan 2016)
9. http://www.cpcb.nic.in/FINAL-REPORT_AQI_.pdf (accessed on 18th Feb 2016)
10. Breathe 2010; 6(3): 234-244
11. BMC Pulm Med. 2014;14:31