Asthma and Pregnancy
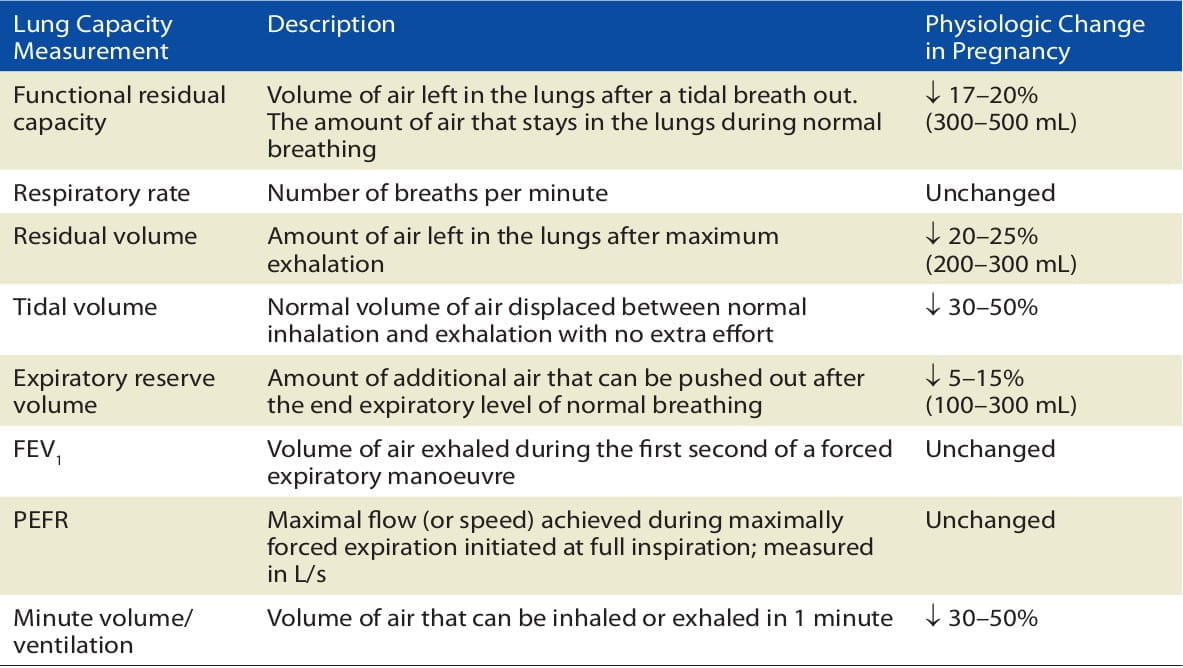
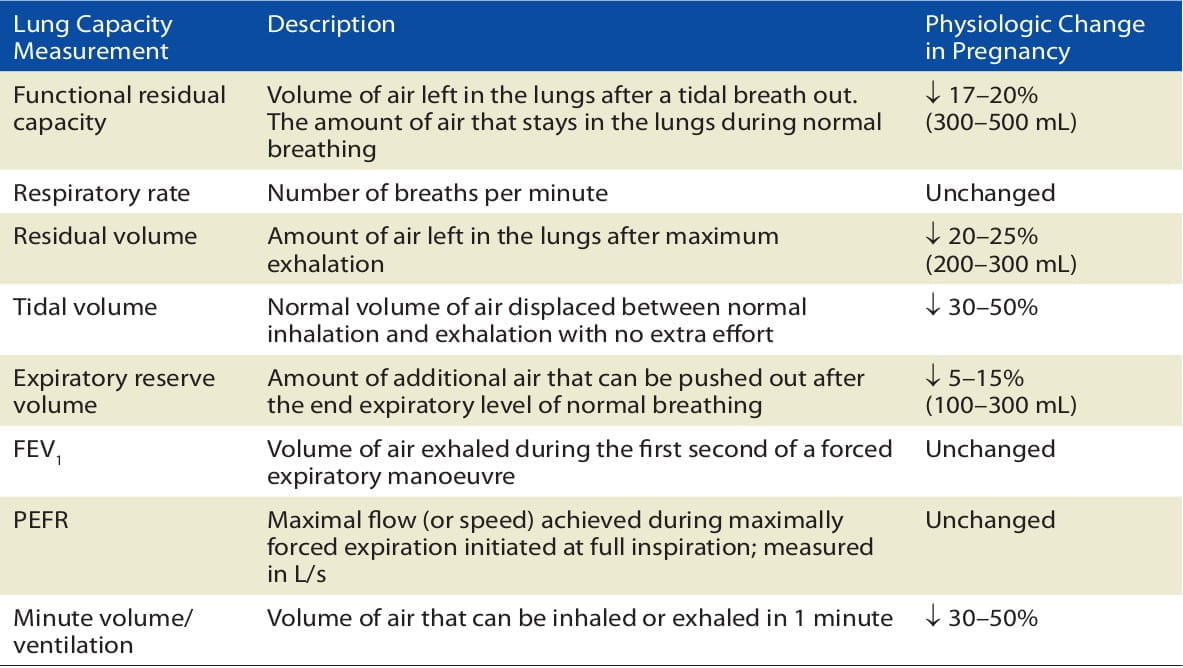
It is a well-known phenomenon that during pregnancy, there is an approximately 18% reduction in the functional residual capacity as well as a progressive decrease in the expiratory reserve volume due to the elevation of the diaphragm for the uterus growth.
Another physiologic change in pregnancy is a 20% increase in the maternal oxygen consumption to support the 15% increase in the maternal metabolic rate. There is also a relative increase in hyperventilation (i.e. 40-50% increase in minute ventilation) to compensate for the increased demands of pregnancy. This natural hyperventilation is a result of increasing tidal volume, and not an increased respiratory rate. Table 1 shows the lung volume descriptions and the respective changes during pregnancy:
Practice Point
Keeping a check on the maternal PaCO2 through an ABG* analysis: The maternal PaCO2 should ideally be low, as an increase in the maternal PaCO2 will affect the ability of the foetus to excrete acid and cause foetal acidosis. Hence, a normal maternal PaCO2 rate in the ABG analysis is actually indicative of a degree of CO2 retention and possible respiratory failure.
* Arterial Blood Gas
Overall, the effect that pregnancy has on any one patient's asthma is unpredictable. Some historical cohort and prospective studies have found that during pregnancy, the severity of asthma remains stable in a third of women, worsens in another third and improves in the remaining third; it is this widely used rule of thirds that makes asthma in pregnancy the very definition of unpredictable!
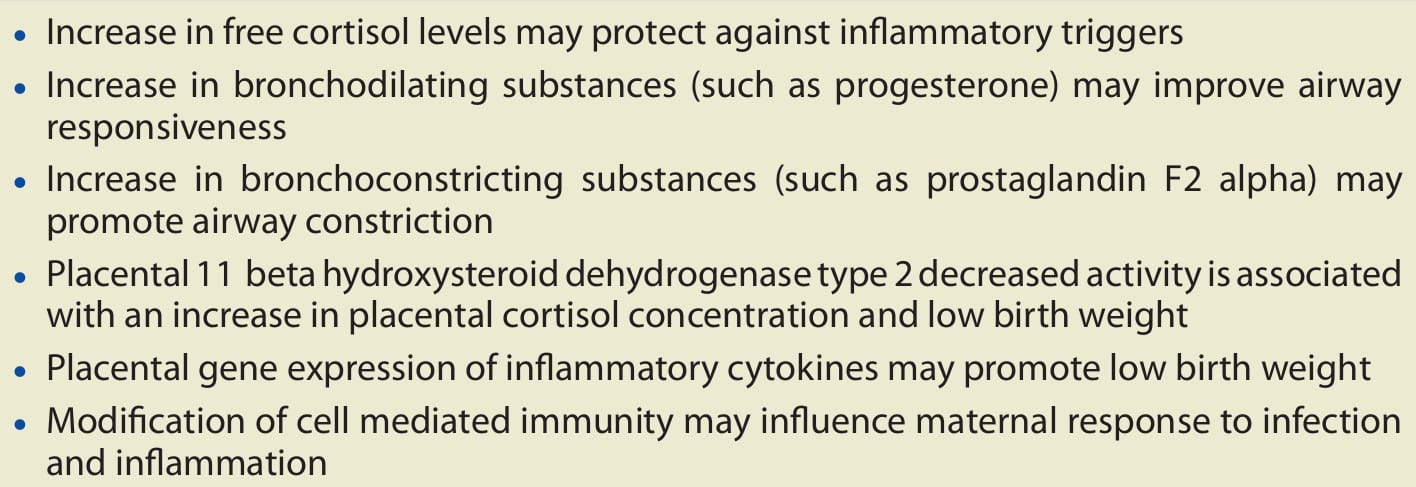
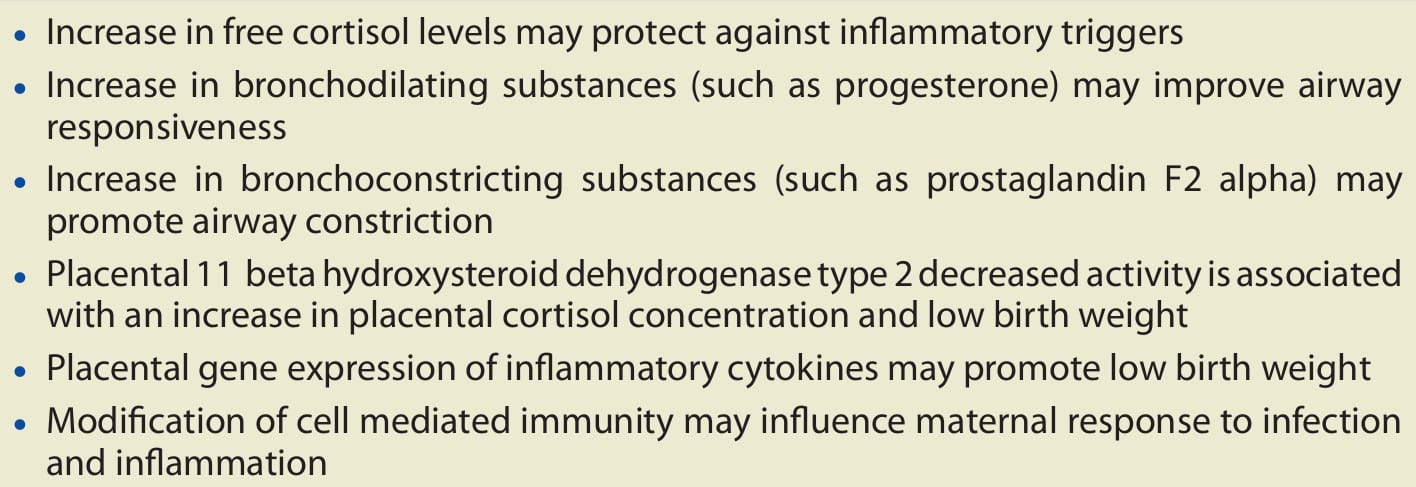
Some of the physiological factors affecting asthma in pregnancy are described below (Box 1):
Exacerbations are most likely to occur between weeks 24 and 36 of pregnancy. Some of the common triggers of exacerbations observed in some studies were respiratory viral infections (34%) and non-adherence to inhaled corticosteroids (29%).
Some studies have also shown that in pregnant women, the condition is more likely to deteriorate in those with severe asthma (52-65%) than in those with mild asthma (8-13%). Also, pregnant women with severe asthma were more likely to have respiratory or urinary tract infections than those with mild asthma or without asthma.
Practice Point
Women with asthma need to be closely followed during pregnancy regardless of the severity of the disease.
There is very little data on how asthma control before pregnancy affects pregnancy outcomes. Also, there is conflicting data on the effects of asthma on pregnancy.
In studies with a large number of pregnant asthmatics, an increased risk of pregnancy induced hypertension has been seen, but only in those with moderate-to-severe daily symptoms. The pregnancy outcomes for asthmatics requiring corticosteroid therapy were associated with decreased gestational age at delivery, pre-eclampsia and small-for-gestational-age infants. However, this data indicates that the poor perinatal outcomes are due to poorly controlled asthma and not because of the treatment medications.
The exact effect of asthma on the developing foetus is poorly understood. Many studies have suggested that maternal hypoxia, inflammation, smoking and altered placental function may contribute to poor outcomes in pregnant asthmatics. However, it is clear that as the asthma worsens or gets more severe, it increases the risk of negative foetal and maternal outcomes.
Practice Point
IT important that asthma is well-controlled before conception and that this control is maintained through continued asthma medication.
Diagnosis of asthma in pregnancy is no different from that in the non-pregnant patient. Asthma is characterized by persistent symptoms of bronchoconstriction, including breathlessness, tightness in the chest, and cough and sputum production. As such, the diagnosis calls for an improvement in the symptoms as well as objective changes in pulmonary function tests such as the FEV1 or PEFR reversibility.
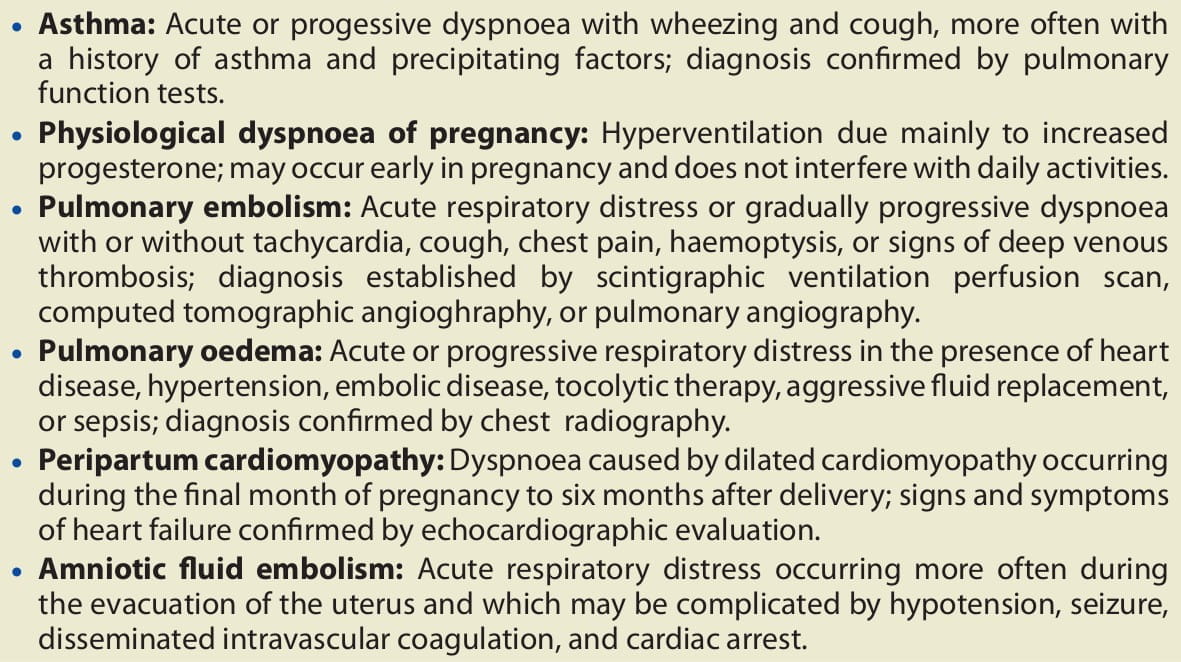
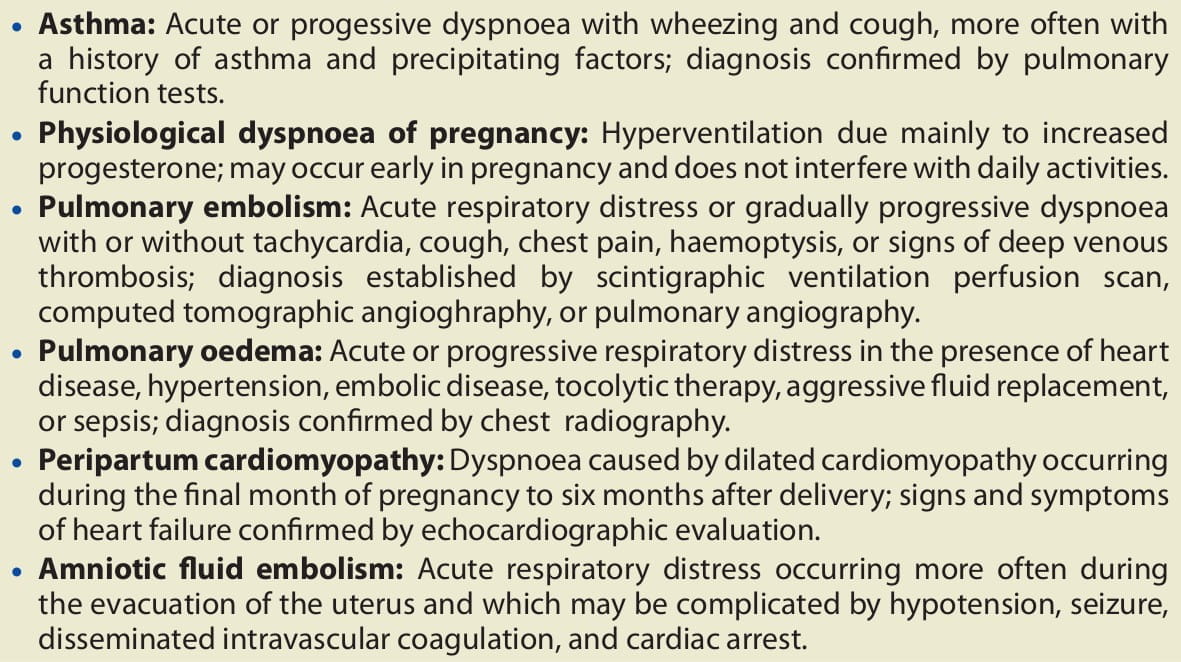
The most common respiratory symptom during pregnancy is dyspnoea without the associated cough, tightness or obstructive signs as seen with asthma; the reason for this dyspnoea is mostly physiological. Hence, an alternate diagnosis such as GERD, pneumonia, post-nasal drip due to allergic rhinitis or bronchitis, etc., may also be considered (Box 2):
Practice Point
If the clinical picture is consistent with asthma but reversibility of airway obstruction cannot be demonstrated, then a trial of asthma treatment can be used for diagnosis in pregnancy.
Once a diagnosis of asthma has been established, it is also important that the asthma severity is classified in a similar way as is usually done in adult asthmatics to help predict the possible risk of severe exacerbations and to establish a regular maintenance therapy. The general principles for the management and treatment of asthma are the same in pregnant women as in non-pregnant women and in men. Knowing and applying the classification system is essential to selecting the appropriate management route as well as anticipating complications during pregnancy.
The ultimate goal of asthma therapy in a pregnant patient is to achieve optimal asthma control for improved maternal and perinatal outcomes. This is expected to be met by preventing hypoxic episodes and preserving continuous foetal oxygenation. Thus, effective asthma management revolves around these four basic components of asthma therapy:
- Assessment and close monitoring of asthma
- Patient education
- Trigger avoidance
- Pharmacotherapy according to severity and control
Since one-third of women with asthma develop worsening of control during pregnancy, it is important that all pregnant asthmatics be closely monitored and re-evaluated.
Since subjective measures used by the patient or physician to gauge the asthma severity are not reliable, objective measurement of the FEV1 with a spirometer (if not available, then measurement of the PEFR with a peak flow meter) is a dependable criterion of airway obstruction and correlates with pregnancy outcomes.
Practice Point
- Women who have sub-optimally controlled asthma or moderate-to-severe asthma (starting at 32 weeks) or who are recovering from a severe asthma exacerbation may be considered for additional foetal surveillance in the form of ultrasound examinations.
- Antenatal surveillance of foetal well-being should be considered in women who have persistent asthma during pregnancy and the intensity of this surveillance should be based on the severity of asthma as well as any other high-risk features of pregnancy that may be present (such as the risk of intrauterine growth retardation and pre-eclampsia).
- Patients should also be instructed to be attentive to foetal activity.
Point to Ponder: Spirometry During Pregnancy
The measurement of the FEV1 after a maximal inspiration (using a spirometer) is the single best measure of pulmonary function even though it is an effort-dependent test. When adjusted for confounders, a mean FEV1 less than 80% predicted has been found to be significantly associated with an increased preterm delivery less than 32 weeks and less than 37 weeks, and a birth weight less than 2,500 gm. Spirometry with pre- and post-bronchodilation is recommended to evaluate the airflow obstruction and reversibility. However, if the spirometry is normal but asthma is highly suspected, a trial of asthma therapy can be initiated for the purpose of diagnosis.
Controlling asthma during pregnancy is important for foetal well-being and, hence, it is recommended that the pregnant asthmatic be imparted more information about asthma.
Practice Point
Patient education should begin at the first prenatal visit and include the following:
- The patient should be made to understand that it is safer to be treated with asthma medications than it is to have asthma symptoms and exacerbations.
- She should be able to recognize and promptly treat the signs of worsening asthma and have prompt access to her clinician in case of uncontrolled symptoms.
- She should be taught how to do peak flow measurements, how to record the results and which values should be of concern, as well as who to contact in emergency.
- She should have a basic understanding of medical management during pregnancy and should be observed using her inhalers as well as peak flow meters, with correct use being reinforced if needed.
- She should also understand what contributes to her asthma severity, i.e. asthma triggers, and how to reduce her exposure or control them.
Identifying and avoiding triggers that contribute to asthma severity can lead to improved maternal well-being, along with less need for medications.
Practice Point
- Identification of triggers in patients can be done either by using skin prick tests or through in vitro tests such as the radioallergosorbent test (RAST) or the enzyme-linked immunosorbent assay (ELISA).
- For exercise-induced asthma, the use of a bronchodilator, 5-60 minutes before exercise, may reduce the symptoms.
- All patients should be strongly encouraged to stop smoking as maternal smoking may be associated with an increased risk for wheezing and development of asthma later on in the offspring.
Point to Ponder: Allergy Treatment and Immunotherapy
Immunotherapy may be continued if the patient is stable on the medication and receiving maintenance doses. Starting immunotherapy or advancing the dose is not recommended during pregnancy due to the risk of anaphylaxis. Allergic rhinitis is a potent trigger of asthma symptoms; pregnancy can worsen the symptoms of allergic rhinitis, resulting in uncontrolled asthma. Allergic rhinitis is generally treated with antihistamines and/or an intranasal corticosteroid. The preferred corticosteroid is budesonide because of the availability of sufficient safety data. However, the overall safety profile of intranasal corticosteroids supports continuing any corticosteroid effective in controlling the patient's symptoms. Recommended antihistamines include first-generation diphenyhydramine and second-generation loratadine, cetirizine and levocetirizine. Decongestants have been associated with an increased occurrence of gastroschisis when taken during the first trimester and should be avoided.
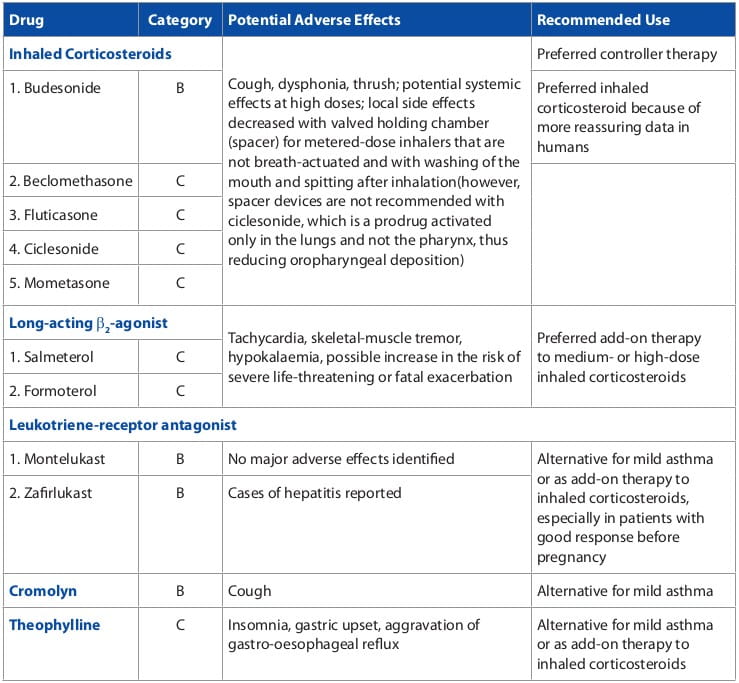
The stepwise approach to therapy, which remains similar to the asthma management in the adults, in which the dosage, number of medications and the frequency of administration are increased as necessary and decreased when possible, is used to achieve and maintain asthma control.
Many pregnant women and their doctors are concerned about the potential effects of the asthma drugs on their babies as well as on the women themselves. It is, however, safer to take asthma drugs during pregnancy than to leave the asthma uncontrolled.
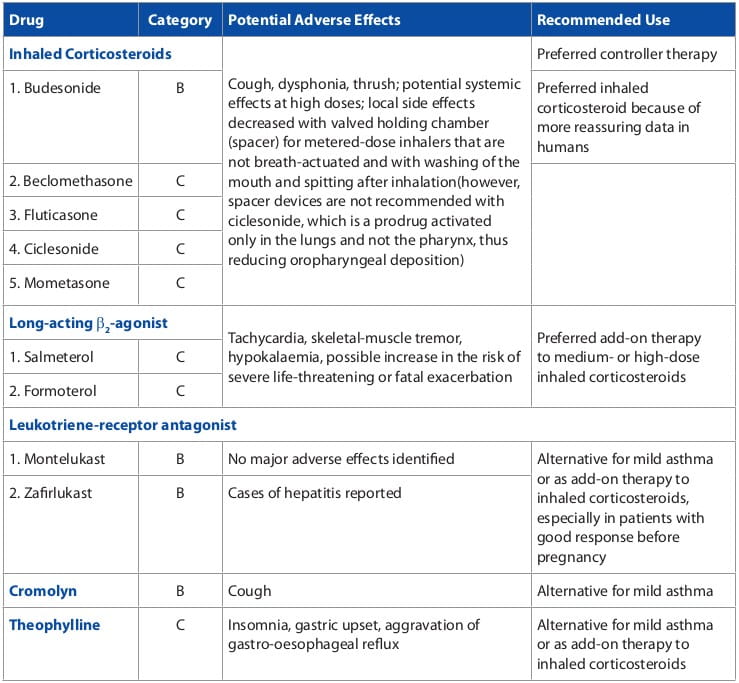
In addition to the animal studies, prospective as well as case-control studies and systematic reviews have shown that asthma drugs such as inhaled corticosteroids, short-acting beta2-agonists and leukotriene-receptor antagonists (such as montelukast) and theophylline, do not increase the risk of foetal congenital malformations, pre- eclampsia, preterm delivery or low birth weight. Long-acting beta2-agonists should always be used together with an inhaled corticosteroid, just as in cases other than pregnancy. In addition, the doctor should not refrain from using oral corticosteroids in severe asthma and life-threatening situations.
It is assumed that asthma medications are as effective in the pregnant asthmatic as in the non-pregnant one; however, there may be physiological changes in pregnancy that affect many aspects of the pharmacokinetics of these medications.
Practice Point
At least twice during the pregnancy, the treatment should be reviewed and stepped up if symptoms are persistent; if they are well-controlled, therapy can be maintained or even decreased.
Point to Ponder: Use of Inhaled Corticosteroids Iin Pregnant Women
Inhaled corticosteroids are preferred for the management of all levels of persistent asthma in pregnancy. Corticosteroids are the most effective treatment for the airway inflammation of asthma and reduce the hyper-responsiveness of the airways to allergens and triggers. They also decrease the incidence of exacerbations by more than threefold in users, compared with those who do not use inhaled corticosteroids. A concern about the risks of congenital malformations with inhaled corticosteroid exposure in the first trimester has proved unfounded; multiple studies have confirmed their safety regardless of dose. In fact, it has been proven that patients with inadequate inhaled anti-inflammatory treatment during pregnancy run a higher risk of an acute attack of asthma, which would then warrant treatment with oral/ systemic corticosteroids, thus increasing the risk of pre-eclampsia. Budesonide is considered the preferred medication because of the availability of sufficient safety data regarding its use in pregnant asthmatics and in the pregnancy category B. All other corticosteroids are category C. However, if a woman's asthma is well-controlled on a different inhaled steroid, it is recommended that the regimen be continued.
An asthma exacerbation in a pregnant woman places her as well as her foetus at increased risk of severe hypoxaemia during these events. The most important part of managing such an event is prevention, but it has also been noted that 52% of patients with severe asthma have an exacerbation during pregnancy and many of them require hospitalization.
A decrease in foetal movement may be an early manifestation of an asthma exacerbation.
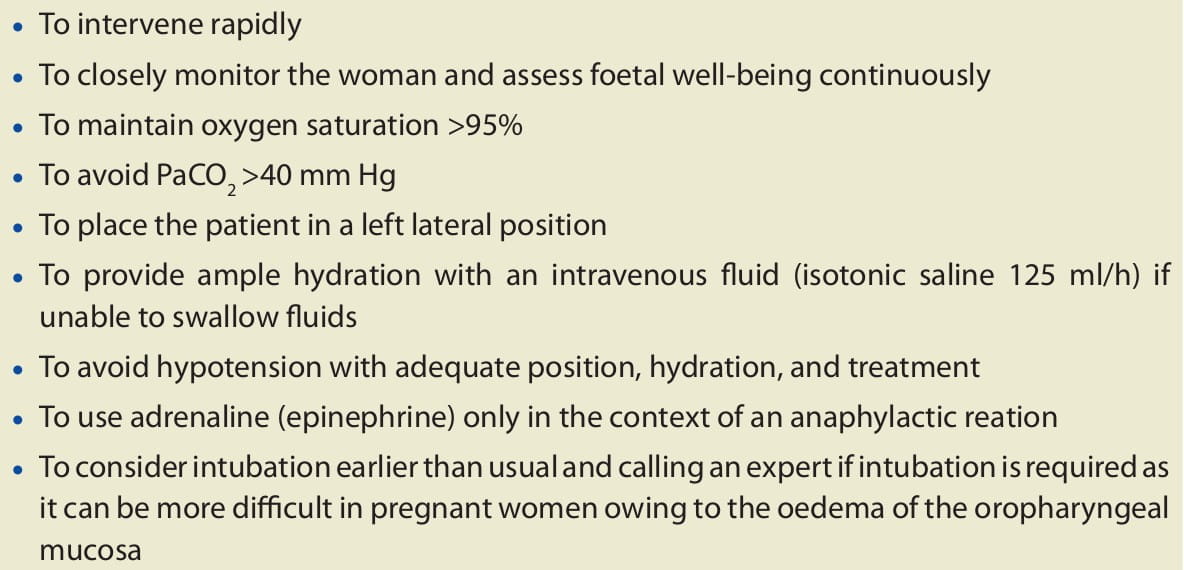
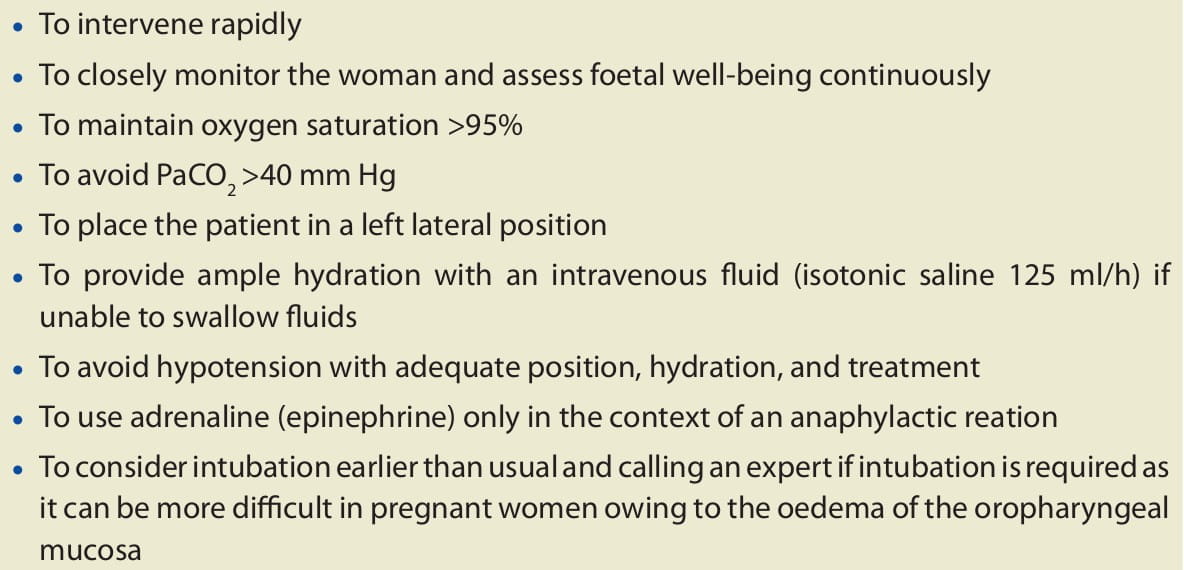
Admission to an intensive care unit, or intubation, is indicated in those with life-threatening asthma, in those with a PaCO2 higher than 40-45 mm Hg on arterial blood gas, mental status changes, maternal exhaustion, respiratory acidosis or foetal distress.
Early recognition of worsening asthma is important so that prompt home rescue treatment may be instituted to avoid maternal and foetal hypoxia; the principles for managing an acute exacerbation of asthma during pregnancy remain the same as in a non-pregnant patient. The goal of hospital management is reversal of bronchoconstriction with inhaled beta2-agonists and corticosteroids, prevention and correction of hypoxaemia, or reduction of hypercarbia. However, there are some precautions to be taken in managing asthma exacerbations in pregnancy (Box 3):
Refractory status asthmaticus is defined as a severe exacerbation of asthma that is unresponsive to bronchodilators and corticosteroids; it requires admission to an intensive care unit and, typically, mechanical ventilation.
Improvement in a severe asthma exacerbation after delivery (if it is being considered) may result from several physiological factors, including reduced pressure on the diaphragm and decreased oxygen consumption.
Practice Point
- Pregnant asthmatics should be taught to recognize the signs and symptoms of early exacerbations, such as coughing, chest-tightness, dyspnoea, wheezing, or a 20% decrease in their PEFR rate.
- Additionally, they should be given an individualized guide for decision making and rescue management .
- However, they should seek further medical attention promptly if the response is incomplete or if foetal activity is decreased.
- In pregnant patients with refractory status asthmaticus, delivery should be considered as a therapeutic option; however, this is rarely required. A caesarian delivery is most likely necessary where there is an urgent need for the delivery.
- Vaginal delivery may be possible during an acute exacerbation in a setting of progressive active labour, normal maternal oxygenation, absence of hypercapnoea, adequate neuraxial anaesthesia, and the use of operative vaginal delivery.
- If delivery is being considered for maternal reasons at a gestational age between 24 and 34 weeks, then betamethasone should be given before the delivery for foetal lung maturity, if at all possible.
- Asthma medications should not be discontinued or delayed during labour and delivery.
- Although asthma during labour is typically quiescent, consideration should be given to obtaining a peak flow measurement on admission and then every 12 hours or as needed to monitor for asthma exacerbation. Monitoring is, more likely, only necessary in those women who have a history of exacerbations during pregnancy.
- Neuraxial anaesthesia decreases the oxygen requirements and minute ventilation and, thus, can be helpful in controlling asthma symptoms during labour.
- If systemic (oral or intravenous) corticosteroids have been used for treatment in the previous 4 weeks, then the patient should receive stress-dose steroids to prevent an adrenal crisis. Usually, this regimen begins with hydrocortisone 100 mg every 8 hours, continued for 24 hours postpartum, and then stopped. Tapering of the dose of stress- steroids is not necessary.
- Medications typically used for tocolysis, induction of labour and during delivery can have an influence on asthma symptoms, especially in the most severe or medication- sensitive asthmatic patients. Prostaglandins E2 or E1 can be used for cervical ripening, for postpartum haemorrhage or to induce abortion without significant adverse reactions. In these cases, the respiratory status of the patient should be routinely monitored. Carboprost (prostaglandin F2-alpha), ergonovine and methylergonovine can cause bronchospasm, especially in the aspirin-sensitive patient. For these patients, choosing a medication such as misoprostol, which is an E1, may be more appropriate.
- Magnesium sulphate is a bronchodilator and should not have a deleterious effect on asthma, but indomethacin can induce bronchospasm in an asthmatic patient with known aspirin sensitivity.
- No formal studies on calcium channel blockers in the gravid asthmatic have been published, but bronchospasm has not been observed with the wide clinical use of these medications for tocolysis.
- It is important to continue asthma medications in the postpartum period.
- Peak flow values should be monitored on the days following delivery in women with moderate-to-severe asthma.
- Breastfeeding should be encouraged since it has been reported that breastfeeding between 1 and 6 months reduces the later prevalence of atopy in 17-year-olds by about 30-50%. However, it does not appear to protect the offspring from developing asthma.
- Even though asthma medications are excreted in small and varying amounts into the breast milk, most asthma medications, including oral prednisone, are considered compatible with breastfeeding.
- Prednisone, theophylline, cromolyn, antihistamines, inhaled corticosteroids or inhaled beta-agonists are not contraindicated during breastfeeding.
- To ensure optimal asthma control throughout pregnancy
- To manage asthma exacebations aggressively
- To avoid delay in diagnosis and treatment
- To assess medication needs and response to therapy frequently
- To ensure adequate patient education and acquisition of self - management skills
- To treat rhinitis, gastric reflux and other comorbidities adequately
- To encourage smoking cessation
- To assess pulmonary function (expiratory flow) with spirometry at least monthly
- To offer a multidisciplinary team approach
- To do not give flu vaccination until after 12 weeks of pregnancy
- To be aware of the risk of pre-eclampsia and intrauterine growth retardation
Asthma is a chronic illness that can complicate a significant number of pregnancies since exacerbations and poor asthma control can have proven negative effects on the pregnancy outcomes. However, with effective treatment and an emphasis on the importance of good asthma control, women with asthma can expect good pregnancy outcomes by ensuring not only their own health but also the health of the growing foetus.
1. National Asthma Education and Prevention Program (NAEPP) - working group report on Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment, Update 2004.
2. Obstet Gynecol Clin N Am 2010; 37: 159-172.
3. Lung India 2007; 24: 33-40.
4. Treat Respir Med 2006; 5(1): 1-10.
5. BMJ 2007; 334: 582-585.
6. N Engl J Med 2009; 360: 1862-9.
7. Obstet Gynecol 2006; 108: 667-81.
8. Dimens Crit Care Nurs 2005; 24(6): 263-266.
9. The Nurse Practitioner 2010; 35 (4).

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)