Asthma is a chronic inflammatory disorder of the airways. The chronic inflammation is associated with airway hyper-responsiveness that leads to recurrent episodes of wheezing, breathlessness, chest tightness and coughing (particularly at night or in early morning).
Asthma in Pregnancy - Your Questions Answered
Asthma in Pregnancy
...Your Questions Answered
What is Asthma?
Is Asthma Common in Pregnancy?
Asthma is the most common, potentially serious medical problem to complicate pregnancy. It is estimated that asthma currently affects 3.7% to 8.4% of pregnant women worldwide.
What are the Physiological Changes in the Respiratory System During Pregnancy?
- Increase in free Cortisol levels may protect against inflammatory triggers
- Increase in bronchodilating substances (such as progesterone) may improve airway responsiveness
- Increase in bronchoconstricting substances (such as prostaglandin F2α) may promote airway constriction
- Placental 11 β hydroxysteroid dehydrogenase type 2 decreased activity is associated with an increase in placental cortisol concentration and low birth weight
- Modification of cell mediated immunity may influence maternal response to infection and inflammation
Does Pregnancy Affect Asthma?
The pregnant patient may develop asthma for the first time during pregnancy. In contrast, in other pregnant patients with pre-existing asthma, the asthma may worsen In a third of women. Improve In another third, or remain unchanged in the remaining third during pregnancy. It is, thus, difficult to predict specifically as to how a patient's asthma may be affected during pregnancy.
Which are the Factors that Worsen Asthma During Pregnancy?
- Pulmonary refractoriness to cortisol effects because of competitive binding to the glucocorticoid receptors by progesterone, aldosterone or deoxycorticosterone
- Prostaglandin F2α-mediated bronchoconstriction
- Decreased functional residual capacity of the lungs
- Increased plasma basic protein reacting in the lungs
- Increased viral or bacterial respiratory infection-triggered asthma
- Increased gastro-oesophageal reflux - induced asthma
- Increased stress
- Reduced PaCO2 (partial pressure of carbon dioxide in arterial blood)
Does Asthma Affect Pregnancy?
Outcomes of pregnancy in asthmatic women have suggested that uncontrolled asthma can have adverse effects on both the mother and foetus which may lead to- increased risk of perinatal mortality, higher rates of pregnancy induced hypertension or pre-eclampsia and caesarean section, vaginal haemorrhage, preterm births and low birth weight infants, neonatal hypoglycaemia and seizures, premature rupture of membranes, transient tachypnea of the new born. Patients with more severe asthma are at a greater risk. If asthma is controlled, these adverse outcomes can be avoided. Thus, pregnant asthmatics should be closely monitored by way of pulmonary function testing during pregnancy.
How is Asthma Diagnosed?
Diagnosis of asthma can lead to a healthier and less risky pregnancy, by decreasing the adverse effects of breathlessness on the developing foetus.
The diagnosis of asthma is based on:
- History
- Physical examination
- Pulmonary function tests
A clinical diagnosis of asthma is often prompted by symptoms such as episodic breathlessness, wheezing, cough and chest tightness. Episodic symptoms after an incidental allergen exposure, seasonal variability of symptoms and a positive family history of asthma or atopic disease are also helpful diagnostic guides.
A good history and clinical examination usually suffice to diagnose asthma in most patients.
Pulmonary function tests like measurement of peak expiratory flow rate (PEFR) with the help of a simple tool called peak flow meter can also aid in the diagnosis of asthma. PEFR is the easiest and most commonly performed test. It is the fastest rale at which air can move through the airways during a forced expiration starting with fully inflated lungs.
The peak flow varies according to age, sex and height. An asthmatic's normal peak flow should be within 20% of that of a person who is of the same age, height and sex, but who does not have asthma.
What are the Main Differential Diagnoses in Pregnant Women with Dyspnoea?
Main Differential Diagnoses in Pregnant Women with Dyspnoea:
- Asthma:- Acute or progressive dyspnoea with wheezing and cough, more often with a history of asthma and precipitating factors; diagnosis confirmed by pulmonary function tests
- Physiological dyspnoea of pregnancy:- Hyperventilation mainly due to increased progesterone; may occur early in pregnancy and does not interfere with daily activities
- Pulmonary embolism:- Acute respiratory distress or gradually progressive dyspnoea with or without tachycardia, cough, chest pain, haemoptysis, or signs of deep venous thrombosis; diagnosis established by scintigraphic ventilation perfusion scan, computed tomographic angiography, or pulmonary angiography
- Pulmonary oedema:- Acute or progressive respiratory distress in the presence of heart disease, hypertension, embolic disease, tocolytic therapy, aggressive fluid replacement, or sepsis; diagnosis confirmed by chest radiography
- Peripartum cardiomyopathy:- Dyspnoea caused by dilated cardiomyopathy occurring during the final month of pregnancy to six months after delivery; signs and symptoms of heart failure confirmed by echocardiographic evaluation
- Amniotic fluid embolism:- Acute respiratory distress occurring more often during the evacuation of the uterus and which may be complicated by hypotension, seizure, disseminated intravascular coagulation, and cardiac arrest
How is Asthma During Pregnancy Managed?
The ultimate goal of asthma therapy in a pregnant woman is to achieve optimal asthma control for Improved maternal and perinatal outcomes. This is expected to be met by preventing hypoxic episodes and preserving continuous foetal oxygenation. Thus, effective asthma management revolves around these four basic components of asthma therapy:
- Assessment and close monitoring of asthma
- Patient education
- Trigger avoidance
- Pharmacotherapy according to severity and control
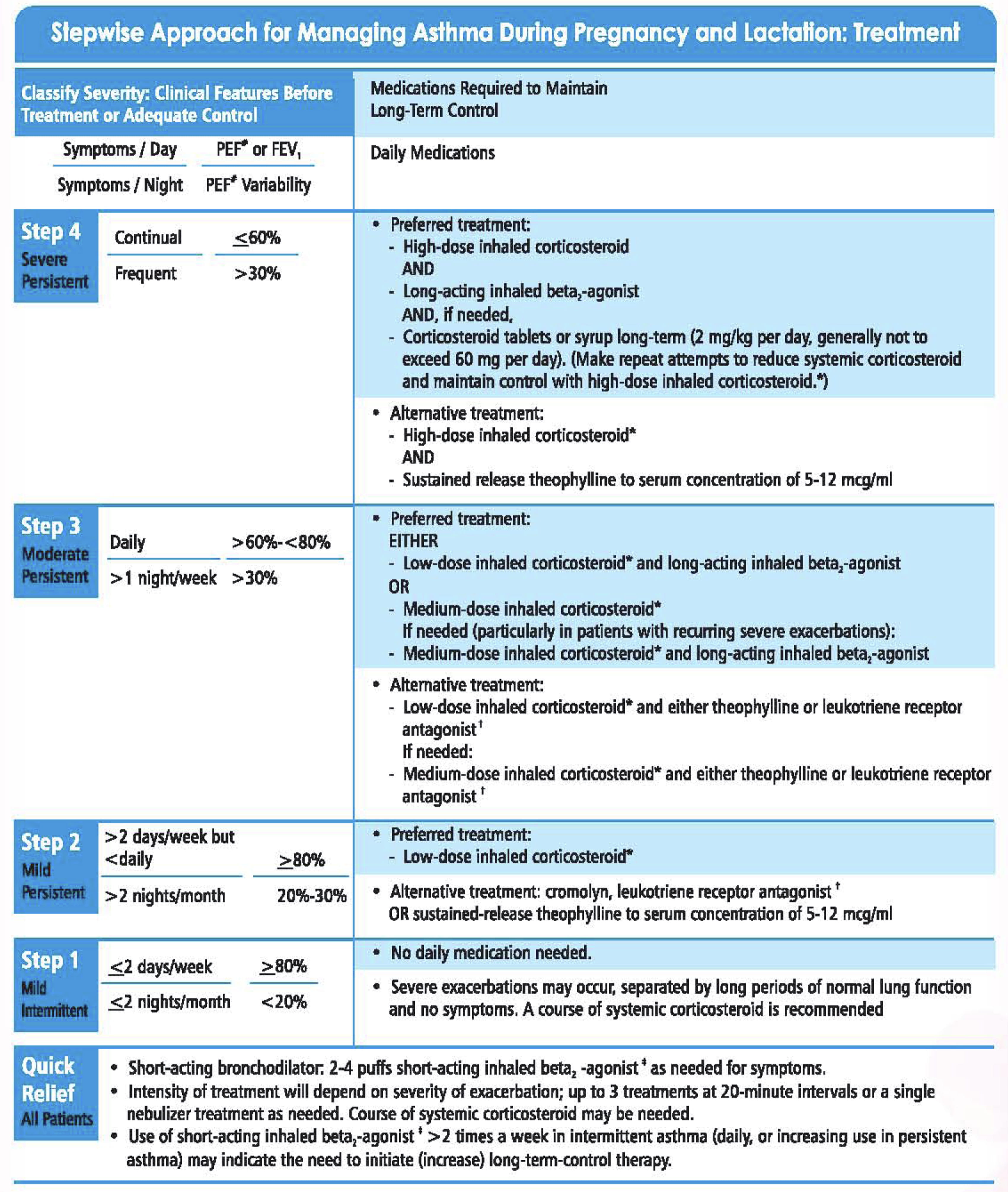
The stepwise approach to therapy, which remains similar to the asthma management in the adults, in which the dosage, number of medications and the frequency of administration are increased as necessary and decreased when possible, is used to achieve and maintain asthma control.
Many pregnant women and their doctors are concerned about the potential effects of the asthma drugs on their babies as well as on the women themselves. It is, however, safer to take asthma drugs during pregnancy than to leave the asthma uncontrolled.
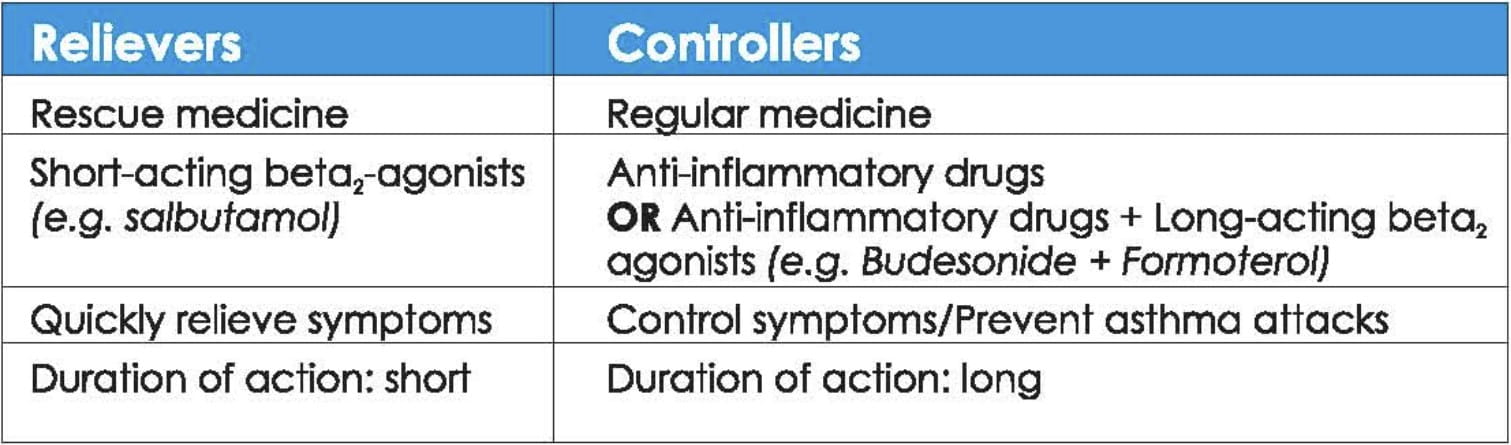
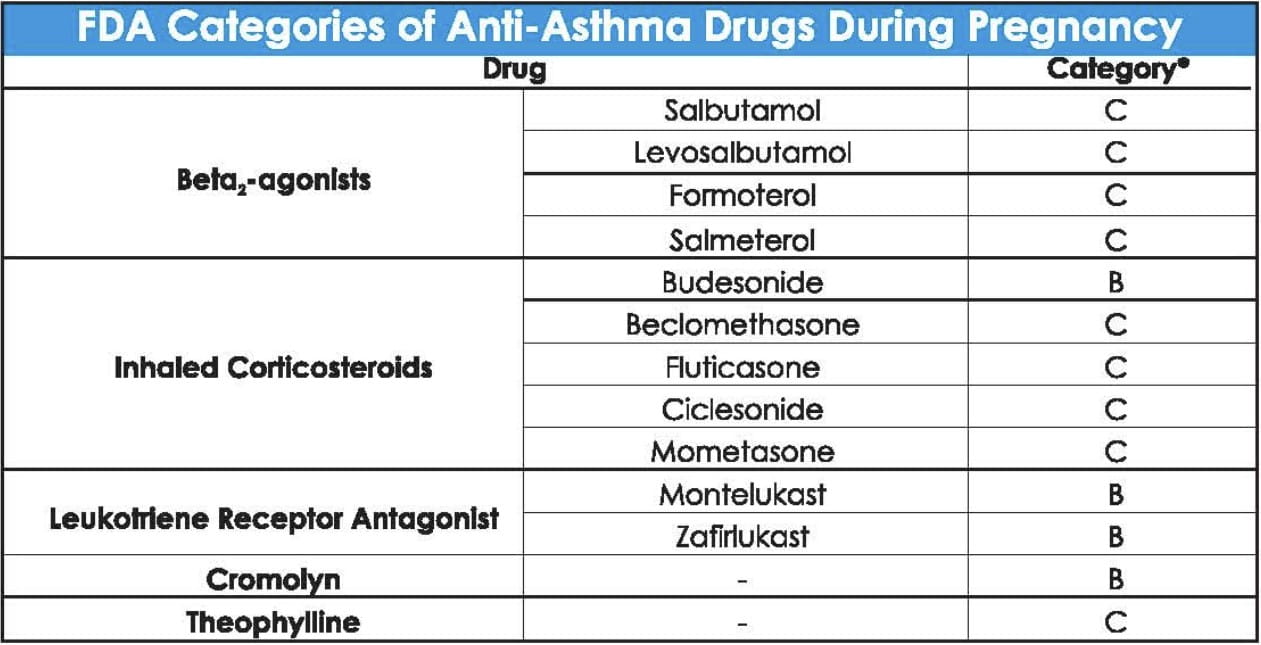
Treatment of the pregnant asthmatics should include medications required for acute symptoms (relievers) and chronic treatment (controllers) as reviewed in the table below:
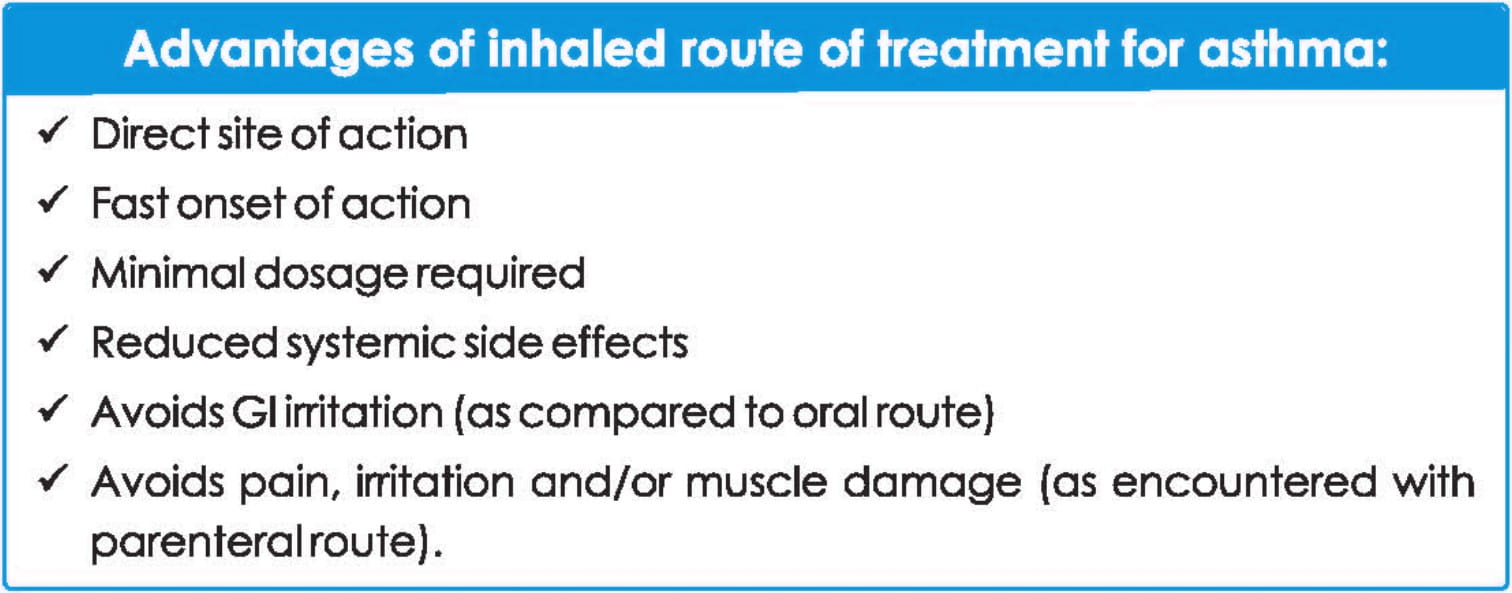
Relievers and controllers can be administered through oral, inhaled and parenteral routes.
However inhalation therapy is the most preferred route of administration and world over most asthmatics are treated with inhaled drugs. Inhaled drug delivery puts the drug where it is needed, whereas oral tablets and syrups must be absorbed in the gastrointestinal tract and need to travel through the bloodstream to various parts of the body before they reach the lungs.
A wide range of inhaler devices are available today which has made inhalation therapy more convenient and accessible.
What is the Importance of Controller Therapy?
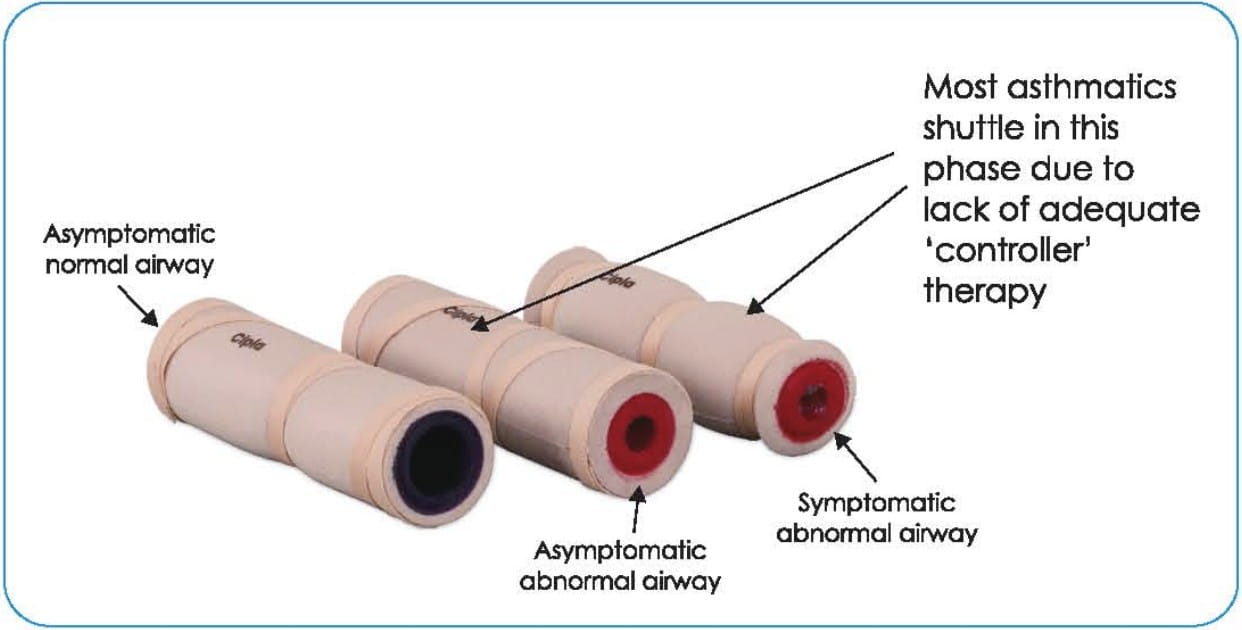
Most asthmatics though asymptomatic have abnormal airways due to underlying inflammation. Without adequate controller therapy, these patients frequently develop symptoms. Thus, they shuttle between asymptomatic and symptomatic state. Adequate controller therapy can restore the airways near to normalcy.
Can Corticosteroids Be Used During Pregnancy?
Corticosteroids are the most effective treatment for airway inflammation of asthma and reduce the hyper-responsiveness of the airways, which decreases the incidence of exacerbations by more than threefold in users, compared with those who do not use inhaled corticosteroids. A concern about the risks of congenital malformations with inhaled corticosteroid exposure in the first trimester has proved unfounded; multiple studies have confirmed their safety regardless of dose. In fact. It has been proven that patients with inadequate inhaled anti-inflammatory treatment during pregnancy are at a higher risk of an acute attack of asthma.
How are Asthma Exacerbations During Pregnancy Managed?
Asthma exacerbations have the potential to lead to severe problems for the foetus. Exacerbations are most likely to occur between 24 and 36 weeks of pregnancy. Therefore, asthma exacerbations during pregnancy should be managed aggressively. A decrease in foetal movement may be an early manifestation of an asthma exacerbation. Hence, the most important part of managing such an event is the prevention of exacerbations.
If the patient experiences dyspnoea due to asthma, successive treatments with a beta2-agonist such as salbutamol should be administered via a pressurized metered dose inhaler (pMDI) or nebulizer. Most of the studies and data available are on salbutamol, whose safety and efficacy is well-established. Evidence to date in animals and humans suggests that beta-sympathomimetics do not increase the risk of congenital abnormalities.
Given below are the steps for the management of an exacerbation presenting in the emergency room:
- Maintain oxygen saturation >95% for foetal well-being
- Administer a short-acting inhaled beta2-adrenoceptor agonist (beta2-agonist) untill improvement of symptoms or evidence of toxicity is noted (e.g. salbutamol metered-dose inhaler with spacer 2-4 puffs OR salbutamol with nebulizer every 10-20 minutes up to three times in succession). Close observation of the patient is necessary with this approach, as use of beta2-agonists may cause tremor and tachycardia and worsen respiratory status by increasing ventilation perfusion mismatches in the lungs
If multiple doses of inhaled beta2-agonists are required or if peak flow and/or FEV1 remain <70% of personal best/predicted:
- Administer methylprednisolone 125 mg intravenously and then 40-60 mg intravenously every 6 hours OR hydrocortisone 200 mg intravenously every 6 hours. No data suggest that one regimen of systemic corticosteroids is better than another, and methylprednisolone and hydrocortisone are simply two corticosteroids that are commonly used
- When there is clinical improvement the patient can be switched to a tapering oral regimen of prednisone (usually 60 mg once daily gradually reduced to nothing over the next 2 weeks)
- Consider the use of ipratropium bromide with nebulizer (2 puffs of 18 mcg spray every 6 hours) or nebulizer (one 0.5 mg vial by nebulizer every 6 hours) during the first 48 hours after presentation
- Position the gravid patient on the left lateral side or with the right hip elevated so that the enlarged uterus does not impair venous return through the inferior vena cava
- Avoid use of subcutaneous epinephrine (adrenaline) in pregnant asthmatic unless it is considered life-saving
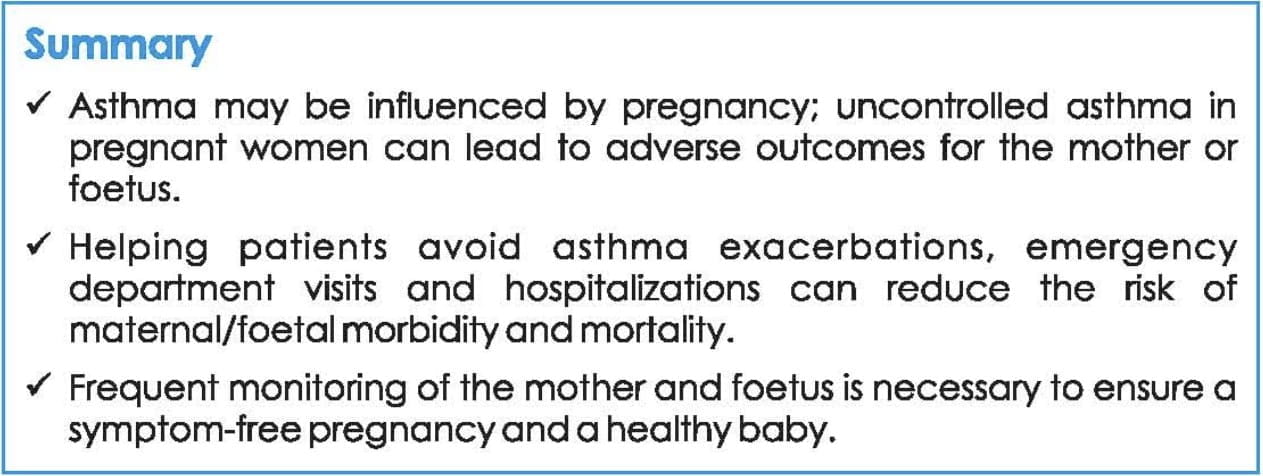
Summary
References
2. Lung India 2007; 24:33-40
3. Treat Respir Med2006; 5(1):1-10
4. BMJ 2007; 334:582-585
5. N Engl J Med 2009;360:1862-9
6. Indian J Allergy Asthma Immunol 2006; 20(2): 117-12
7. Am J Obstet Gynecol 2005; 192:369-80
8. http://www.medscape.com/viewarticle/496583 (Accessed on 18thAugust 2009)
9. http://www.medscape.com/viewarticle/722310 (Accessed on 2ndJune, 2011)