Introduction
The classical symptoms of gastroesophageal reflux disease (GERD) include heartburn and regurgitation. In many patients the presence of these symptoms are suggestive of GERD. However, often, it is difficult to distinguish symptoms of GERD from those of functional gastrointestinal disorders. This is why clinicians do not always rely solely on symptoms. Instead a variety of tests including invasive methods and symptomatic responses have been used to evaluate patients with GERD. From the array of choices available the clinician will carefully select the test the patient may require. The detailed list of tests is mentioned below.
Questionnaires
Current guidelines recommend diagnosis based on symptoms unless alarm symptoms like dysphagia, weight loss or haemorrhage exist. A validated set of questions is helpful to diagnose patients with GERD. The following questions are helpful to guide a clinician’s conversation with a GERD patient. The answers to these questions are scored and the total of these scores would help a doctor decide if the person is suffering from GERD.
|
|
|
Frequency score (points ) for symptom |
|||
|
|
Variable question |
0 day |
1 day |
2-3 days |
4-7 days |
|
1. |
How often did you have a burning feeling behind your breastbone (heartburn)? |
0 |
1 |
2 |
3 |
|
2. |
How often did you have stomach contents (liquid or food) moving upwards to your throat or mouth (regurgitation)? |
0 |
1 |
2 |
3 |
|
3. |
How often did you have a pain in the centre of the upper stomach? |
3 |
2 |
1 |
0 |
|
4. |
How often did you have nausea? |
3 |
2 |
1 |
0 |
|
5. |
How often did you have difficulty getting a good night’s sleep because of your heartburn and ⁄ or regurgitation? |
0 |
1 |
2 |
3 |
|
6. |
How often did you take additional medication for your heartburn and ⁄ or regurgitation, other than what the physician told you to take? |
0 |
1 |
2 |
3 |
|
Interpretation of results (after adding the score for the responses received) |
|
|
Score < 8 |
low probability for GERD |
|
Score ≥ 8 and ≤ 3 on questions 5 and 6 |
GERD with low impact on daily life |
|
Score ≥ 8 and ≥ 3 on questions 5 and 6 |
GERD with high impact on daily life |
Empiric PPI Trial
- Many clinicians use the patient response to PPI therapy as a diagnostic tool for presence of GERD.
- Generally, a short course of a PPI (once daily for 2 weeks) is considered enough to support a diagnosis of GERD. This test is useful to distinguish GERD when symptoms of non-cardiac chest pain are present.
- However, PPI trial has limited utility in patients with erosive esophagitis.
- Patients who do not respond to PPI therapy should be evaluated using other tests like pH monitoring or endoscopy.
Endoscopy
The best way to diagnose erosive reflux disease is through upper gastrointestinal endoscopy. However, endoscopy is not necessary in all patients. The clinical guidelines committee of the American College of Physicians recommended the use of endoscopy in the following situations:
- Heartburn and alarm symptoms (dysphagia, bleeding, anaemia, weight loss, recurrent vomiting).
- Typical GERD symptoms that persists despite a therapeutic trial of 4 to 8 weeks of twice-daily proton-pump inhibitor (PPI) therapy.
- Severe erosive esophagitis after a 2-month course of PPI therapy to assess healing and rule out Barrett’s esophagus.
- A history of esophageal stricture with recurrent symptoms of dysphagia.
- Men >50 years with chronic GERD symptoms (>5 years) and additional risk factors (nocturnal reflux symptoms, hiatal hernia, elevated body mass index, tobacco use, intra-abdominal distribution of fat) to detect esophageal adenocarcinoma and Barrett’s esophagus.
- Surveillance evaluation in men and women with a history of Barrett’s esophagus. In the absence of dysplasia, surveillance examinations should occur at intervals no more frequently than 3 to 5 years. More frequent intervals are indicated in patients with Barrett’s esophagus and dysplasia.
How Should the Patient be prepared for Endoscopy?
- The patient should be fasting for at least 6 hours or more before the start of the procedure.
- Patient should inform the doctor about his medical history. This will help the doctor to assess the need for any other medications required during or after the procedure.
- Patient will be given a topical anaesthetic to numb the throat before inserting the endoscope.
Histology
Histology is useful in diagnosing Barrett`s epithelium and to exclude eosinophilic esophagitis.
pH Monitoring
Esophageal pH monitoring is a test that measures how often stomach acid enters the esophagus. The test also measures how long the acid remains in the esophagus. The gold standard for diagnosing pathologic acid reflux is ambulatory intra- esophageal pH monitoring. It can be done using catheter based pH monitoring system or catheter free pH monitoring system (wireless pH capsule). It is indicated in the following conditions:
- To confirm a diagnosis of GERD before fundoplication
- If symptoms exist after anti-reflux surgery
- In case of extra-esophageal complications
How to Prepare the Patient for the Test?
- Avoid eating or drinking for 12 hours before the test.
- Following medications can affect the results of pH monitoring:
Adrenergic blockers (drugs that relax the muscles of your bladder and prostate), anticholinergics (drugs used in the treatment of spastic GI tract disorders), certain antacids, alcohol, cholinergics (drugs that produce the same effects as the parasympathetic nervous system), corticosteroids (steroid hormones), H2 blockers (drugs used to block histamine effects on your stomach, such as Zantac), proton pump inhibitors (drugs used to reduce gastric acid production).
A major disadvantage of pH monitoring is that there are no absolute values to define GERD in patients undergoing this procedure.
Esophageal Manometry
Esophageal manometry measures contractions in the esophagus and in the lower esophageal sphincter. This test is not required for routine diagnosis of GERD. In some patients where it is difficult to diagnose GERD despite using endoscopy, manometry may be useful. This test helps to correlate reflux episodes with symptoms. Every time the lower esophageal sphincter relaxes, it is recorded. And if this period of relaxation correlates with the time that a patient experiences symptoms, it suggests that the person has GERD.
What are the Precautions to be taken before Esophageal Manometry?
- It is important to tell the doctor if the patient is pregnant, has a lung or heart condition or any other underlying disease.
- If the patient suffers from any allergic reaction due to medications.
- Patient should not eat or drink 8 hours before the procedure.
Radiology
Radiology (barium esophagogram) is an inexpensive and non-invasive procedure for diagnosing GERD. When the organs of the GI tract are covered with barium, the anatomy of the organs including the esophageal structure and presence of hiatal hernia is possible to visualize. It is generally not used to make a diagnosis of GERD but to confirm presence of esophageal structural lesions or hiatal hernia. Most patients with GERD symptoms have a normal endoscopic diagnosis and are thought to experience non erosive reflux disease (NERD).
What could be The Risks Involved during This Procedure?
It is usually a safe procedure. However, there can be some of the following complications.
- Allergic reaction to barium
- Constipation
- Aspiration (Barium gets into the windpipe)
What Are The Steps Involved during This Procedure?
- 1-1.5 cups of drink containing barium will be given to the patient. It is likely that children would drink less compared to adults.
- The entire procedure takes about 30-60 minutes to complete.
- The patient is strapped on a table and x-rays will be taken as the barium liquid goes down the digestive system. Some pressure may be applied to the stomach to help spread the liquid throughout.
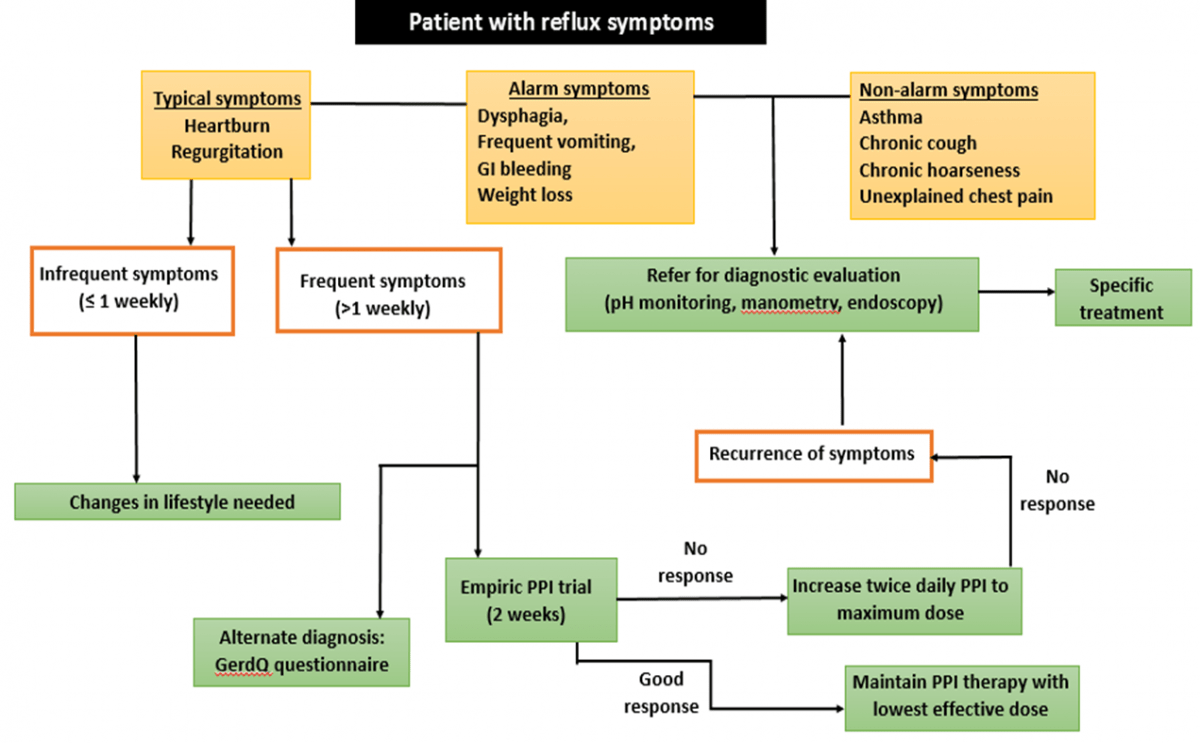
Algorithm for Diagnosis of GERD
References
- Lacy BE et al. The diagnosis of gastroesophageal reflux disease. Am J Med. 2010 Jul; 123(7):583-92.
- Nicholas J. Shaheen et al. Upper Endoscopy for Gastroesophageal Reflux Disease: Best Practice
- Shaheen NJ et al. Advice From the Clinical Guidelines Committee of the American College of Physicians. Ann Intern Med. 2012; 157:808-816.
- Philip O. Katz et al. Diagnosis and Management of Gastroesophageal Reflux Disease. Am J Gastroenterol 2013; 108:308–328.
- http://tidsskriftet.no/pdf/pdf2013/43-6eng.pdf Last accessed on 29/07/2016
- https://medlineplus.gov/ency/article/003401.htm Last accessed on 18/07/2016
- http://www.webmd.com/heartburn-gerd/guide/esophageal-manometry Last accessed on 18/07/2016
- http://www.emedicinehealth.com/barium_swallow/article_em.htm Last accessed on 18/07/2016
- http://www.vzradiology.com/index.php?option=com_content&view=article&id=82&Itemid=430 Last accessed on 18/07/2016
- http://img.medscape.com/fullsize/migrated/editorial/journalcme/2007/8233/richter.fig1.gif Last accessed on 18/07/2016