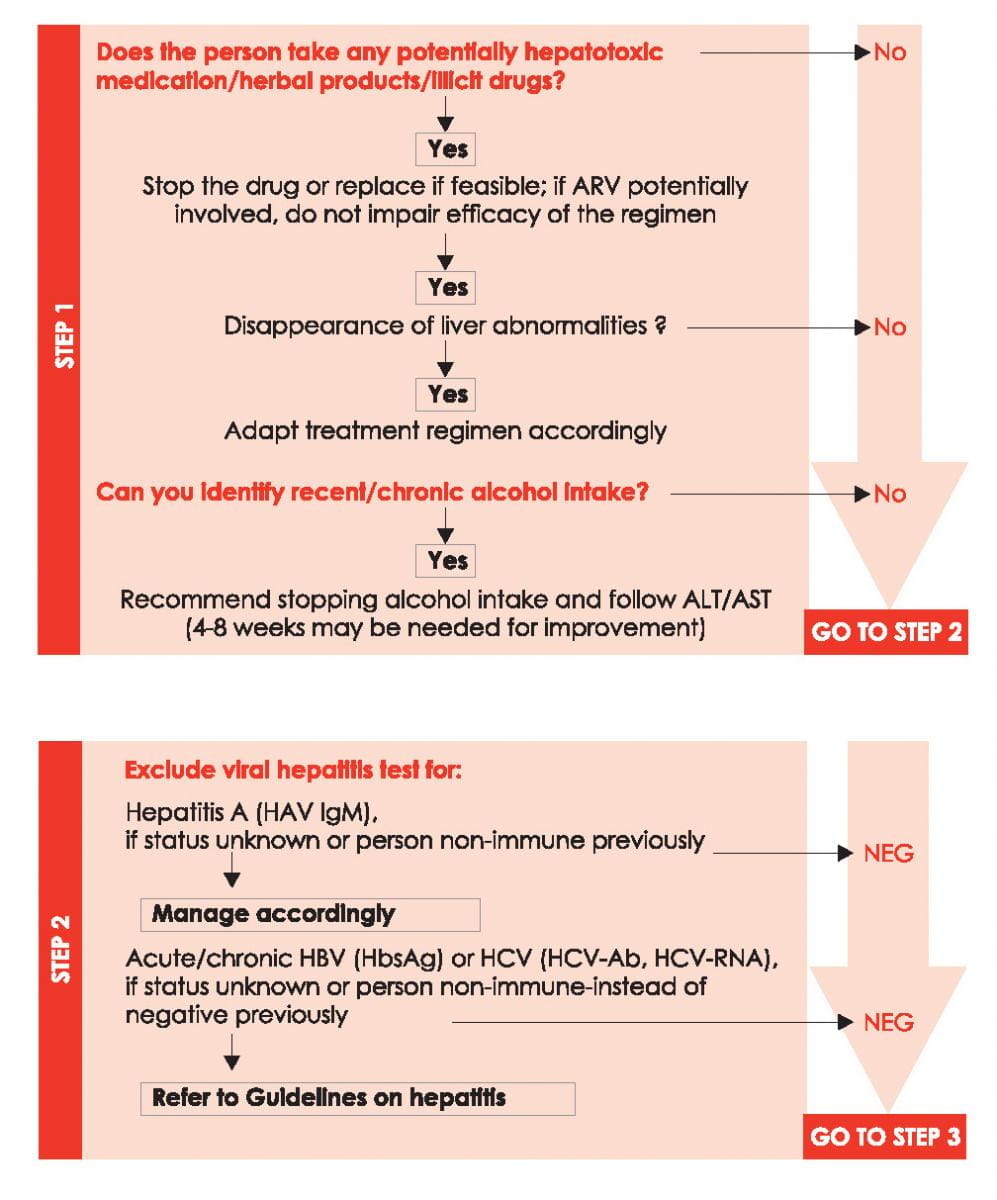
Work-up and Management of HIV-positive Persons with Increased ALT/AST
Identify potential cause of increased liver enzymes, using the following steps:
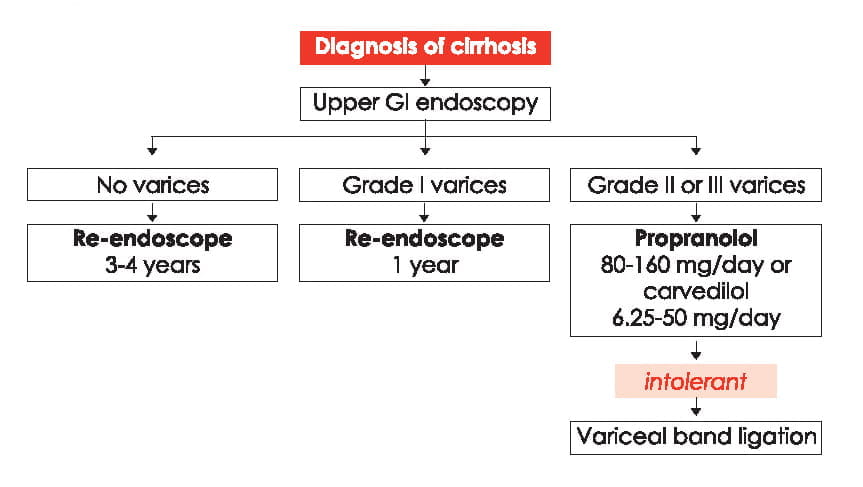
Liver Cirrhosis: Classification and Surveillance
|
Child-Pugh classification of the severity of cirrhosis | |||
|
|
Point (*) | ||
|
1 |
2 |
3 | |
|
Total bilirubin, mg/dL (?mol/L) |
<2 (<34) |
2-3 (34-50) |
>3 (>50) |
|
Serum albumin, g/L (?mol/L) |
>35 (>507) |
28-35 (406-507) |
<28 (<406) |
|
INR |
<1.7 |
1.7-2.20 |
>2.20 |
|
Ascites |
None |
Mild/Moderate (diuretic responsive) |
Severe (diuretic refractory) |
|
Hepatic encephalopathy |
None
|
Grade I-II (or suppressed with medication) |
Grade III-IV (or refractory) |
i5-6 points: Class A
7-9 points: Class B
10-15 points: Class C
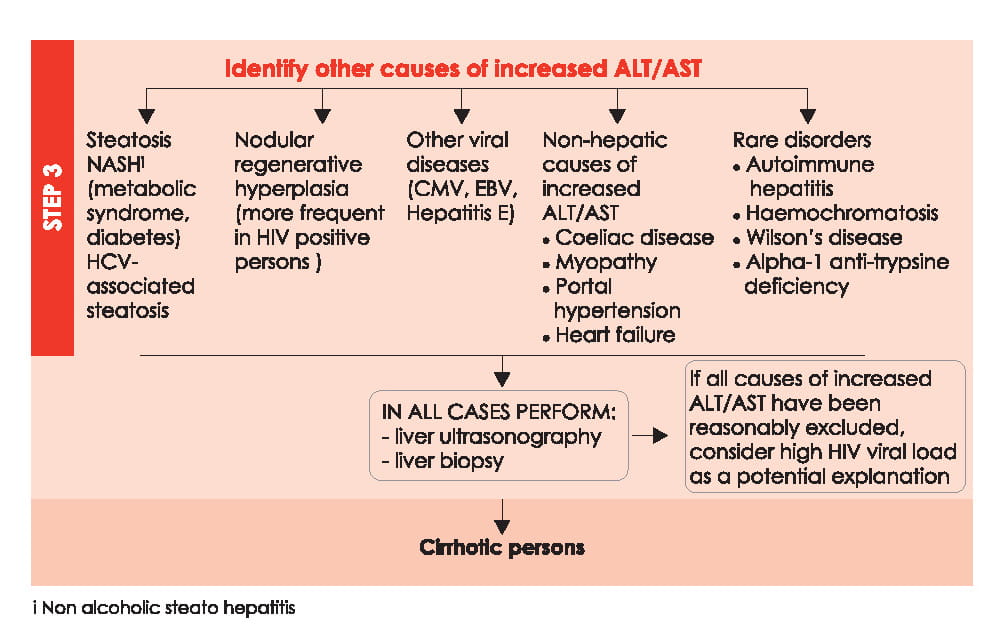
Algorithm for Surveillance for Varices and Primary Prophylaxis
Liver Cirrhosis: Management
Management of HIV-positive persons with cirrhosis should be done in collaboration with experts in liver diseases. More general management guidance is described below.
For dosage adjustment of antiretrovirals, see Dose Adjustment of ARVs for Impaired Hepatic Function.
In end-stage liver disease (ESLD), use of EFV may increase risk of CNS symptoms. ART, if otherwise indicated, also provides net benefit to cirrhotic persons. See Diagnosis and Management of Hepatorenal Syndrome (HRS).
|
Management of hypervolaemic hyponatraemia | ||
|
1. Fluid restriction: 1000-1500 mL/day (consumption of bouillon allowed ad libitum) 2. If fl uid restriction is ineffective, consider use of oral tolvaptan a. To be started in hospital at 15 mg/day for 3-5 days, then titrated to 30-60 mg/day until normal s-Na; duration of treatment unknown (efficacy/safety only established in short-term studies (1 month)) b. S-Na should be monitored closely, particularly after initiation, dose modification or if clinical status changes. c. Rapid increases in s-Na concentration (>8 mmol/day) should be avoided to prevent osmotic demyelisation syndrome d. Persons may be discharged after s-Na levels are stable and without need to further adjust dose | ||
|
Management strategy of hepatic encephalopathy (HE) | ||
|
General management 1. Identify and treat precipitating factor (GI haemorrhage, infection, prerenal azotaemia, constipation, sedatives) 2. Short-term (< 72 hours) protein restriction may be considered if HE is severe Specific therapy Lactulose 30 cm³ orally every 1-2 h until bowel evacuation, then adjust to a dosage resulting in 2-3 formed bowel movements per day (usually 15-30 cm³ orally bid). Lactulose enemas (300 cm³ in 1L of water) in persons who are unable to take it orally. Lactulose can be discontinued once the precipitating factor has resolved. | ||
|
Management strategy in uncomplicated ascites | ||
|
General management |
| |
|
Specific management |
| |
|
Follow-up and goals |
| |
|
Nutrition of cirrhotic persons | ||
|
Caloric requirements
Protein requirements
|
Micronutrients
| |
|
Analgesia in persons with hepatic failure | ||
|
| |
|
Screening for hepatocellular carcinoma | ||
| ||
|
When to refer for liver transplantation? Best to refer early as disease progresses rapidly | ||
|
= MELDii score 10-12 (listing at 15) Decompensated cirrhosis (at least one of the following complications)
| ||
iAlpha-foetoprotein may also be expressed in ?g/L (cut-off value of 400 is the same)
iiUnit for both S-creatinine and S-bilirubin is mg/dL. MELD Score = 10 {0.957 Ln (serum creatinine (mg/dL)) + 0.378 Ln (total bilirubin (mg/dL)) + 1.12 Ln (INR) + 0.643}
Diagnosis and Management of Hepatorenal Syndrome (HRS)
|
Diagnosis |
Consider HRS in a person with cirrhosis and ascites and a creatinine level of >1.5 mg/dL. It is a diagnosis of exclusion. Before making the diagnosis, the following need to be ruled out and treated:
Diuretics should be discontinued and intravascular volume expanded with intravenous (iv) albumin. If renal dysfunction persists despite above, diagnose HRS. | ||
|
Recommended therapy |
Liver transplant (priority dependent on MELD score). If person is on transplant list. MELD score should be updated daily and communicated to transplant centre. | ||
|
Alternative (bridging therapy) |
Vasoconstrictors |
octreotide |
100-200 mcg subcutaneously t.i.d |
|
→ Goal to increase mean arterial pressure by 15 mm hg | |||
|
+ midodrine |
5-15 mg orally tid | ||
|
or terlipressin |
0.5-2.0 mg iv every 4-6 hours | ||
|
and iv albumin (both for at least 7 days |
|
50-100 g iv qd | |
Reference
EACS Guidelines version 8.0 - October 2015