Introduction
Inhalation is the preferred route for administering drugs in the treatment of respiratory diseases such as asthma and chronic obstructive pulmonary disease (COPD).This form of therapy refers to the delivery of the drug directly into the airways with rapid onset of action and minimal systemic adverse effects.If used appropriately by the patients, inhalation devices such as pressurized metered dose inhalers (pMDIs),dry powder inhalers (DPIs),breath actuated inhalers (BAIs) and nebulizers are equally effective. However, there are some important differences in the convenience with which each device is used.
In routine clinical practice, errors with handheld inhalers are commonly seen which can result in inadequate symptom relief. Effective drug delivery with a nebulizer is less technique dependent compared to pMDIs and DPIs and requires less patient training regarding usage.This therapy is particularly well suited for the treatment of airway diseases in children and the elderly.
Of all the aerosolized drug delivery systems, nebulizers are the easiest for the patients to use,requiring minimal cognitive abilities and virtually nohand-breath co-ordination. Also, the mist generated by nebulizers may foster confidence in patients,providing visible evidence that they are receiving the medication. They are widely used to deliver all types of medications including corticosteroids,mucolytics,?2-agonists,anticholinergics and antibiotics.
The nebulizer is a device which converts the liquid drug into a continuous fine aerosol mist,which can be easily inhaled by the patients (via a face mask or a mouthpiece) for both emergency treatment of acute respiratory illness and long-term home treatment,especially in asthma and COPD.The nebulizers are driven by a compressor (electric/battery operated) or oxygen and the patients can breathe normally over a 5-10 minute treatment period.
There are certain disadvantages associated with using nebulizers including poor portability, associated cost, and the need for daily cleaning and proper maintenance. Despite these,the nebulizers have been used clinically for many years and will continue to be used in selected patients with the most important advantage being convenience of use. A number of factors affect nebulizer performance,and these should be considered by the healthcare professionals and patients who use these nebulizers.
Nebulization: Clinical Indications
- Patients too sick or incapable of managing hand held inhalers
- Drugs not available in hand held inhalers
- Need for a large drug dose
- Patient preference
- Practicalconvenience
Using the Nebulizer Correctly
1. Place the compressor on a sturdy surfacesothat the rubber padsarerestingonit.
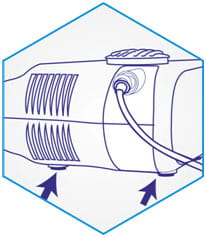
2. Plug the power cord into the electrical outlet.
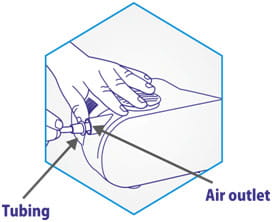
3. Connect one end of the nebulizer tubing to the compressor air outlet.
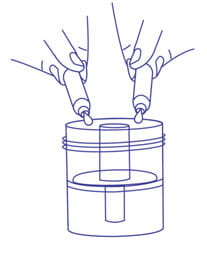
4. Open the cap of the medication chamber.
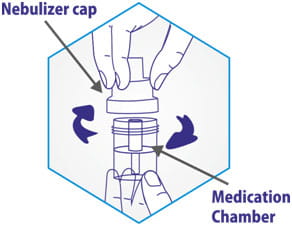
5. Add the medication into the chamber. Re-attach the cap.
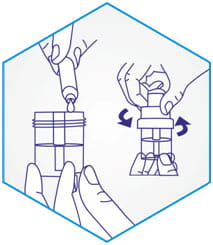
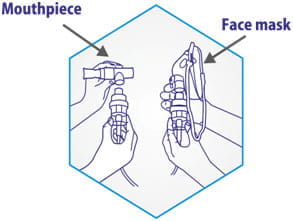
6. Attach the mouthpiece/face mask to the cap of the medication chamber and connect the tubing at the bottom of the medication chamber.
7. Switch on the compressor.

8. If using a mouthpiece, keep it between the teeth and place the lips around it.

OR
8. If a mask is used, place the mask over the mouth and nose.

Inhale deeply and slowly through the mouth and then exhale slowly.
Continue to breathe through the face mask/mouthpiece for the duration recommended.
9. When the treatment is complete, turn the switch off.
For more information, please refer the manufacturer’s user manual.
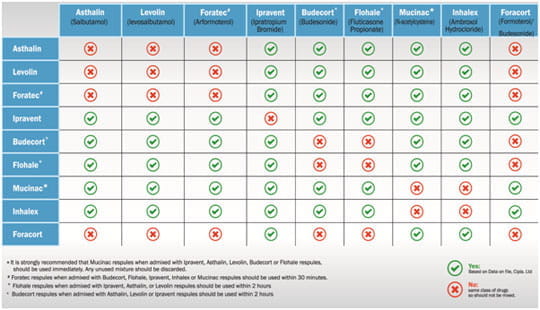
Drug Compatibility
Can a mixture of two drugs be used for nebulization?
Continuous v/s Intermittent Nebulization

Continuous aerosolized bronchodilators are occasionally used in the treatment of acute asthma. The duration of action of inhaled (?2-agonists is short and requires frequent administration. This is thought to dilate the proximal bronchial tree, thereby allowing further distal deposition of subsequent bronchodilator treatments, which produces sustained bronchodilation. All these benefits might be obtained with continuous nebulization of bronchodilators. Typical doses for continuous nebulization (e.g.salbutamol) range from 5 to 15 mg/hr.
Continuous and intermittent nebulization have shown to increase peak expiratory flow by 30% ± 18% and 32% ± 22% respectively; (P< 0.01 over baseline) at the six hour. In this study, 42 acute severe asthmatics (presenting in emergency department) were randomly assigned to receive 27.5 mg salbutamol by either continuous or intermittent nebulization. The continuous nebulization group received
15 mg of salbutamol during the first hour and 12.5 mg over the next 5 hours. The intermittent nebulization group received 5 mg of salbutamol every 20 minutes during the first hour and 2.5 mg hourly over the next 5 hours.
A meta-analysis of continuous vs intermittent nebulization of ?2-agonists in 165 trials supports the use of continuous nebulization in patients with severe asthma presenting in emergency department, which increases the pulmonary function and reduces hospitalizations. However a greater decrease in the heart rate with continuous nebulization has been reported.
A practical approach may be to identify patients who fail to respond to initial treatment with ?2-agonists or those with severe airflow limitation and provide continuous nebulization.
Continuous nebulization therapy is an important means of treating patients with severe asthma. The choice of delivery method should reflect practice situations and economical considerations.
When to Use a Face Mask and a Mouthpiece?
- Drugs can be delivered via a nebulizer using either a mouthpiece or a face mask. However, it is important to instruct the patient to inhale through the mouth.
- The bronchodilator responses are reduced by nearly 50% when the drug is delivered to the lungs via nasal inhalation (since nasal passages effectively filter the droplets delivered from the nebulizer).
- Additionally, use of the mouthpiece has shown a significant increase in the percent FEV1 (56.4%) compared to a face mask (28.9%), as observed in 18 children (aged 8-15 years) with mild-to-moderate asthma exacerbations.
- The incidence of adverse events observed in 481 infants and young children (aged 6 months to 8 years) with moderate persistent asthma was higher (85%) in patients receiving nebulized budesonide via a face mask than those receiving treatment via a mouthpiece (78%).
- Significant facial and eye deposition of aerosol can occur with a face mask particularly when anticholinergics are administered, and can result in blurring of vision, pupil dilation, and worsening of glaucoma.
Mouthpiece should be preferred if delivering:

- Nebulized steroids and antibiotics (to avoid administration on facial skin and into the eyes)
- Anticholinergics (in patients with glaucoma)
Face mask should be used in:

Acutely ill patients, babies and young children who find it difficult to co-ordinate with the mouthpiece
Essential Points to Be Considered During Nebulization
Nebulization Time
- Nebulization time is the time from the start of the nebulization until continuous nebulization has ceased, which is generally 5-10 minutes.
- A short nebulization time that delivers an effective dose is desirable.
Nebulization Fill Volume
- The nebulizer fill volume is usually 2-5 ml (or as recommended by the manufacturer).
- The nebulizer output and time increases with a greater fill volume. When a larger fill volume is used, the nebulization time can be reduced by increasing the flow of nebulizer.
Nebulization End Point
- A 'spluttering' sound indicates the nebulization end point. Tapping the medication chamber when the medication begins to'splutter'may increase the medication output by upto 50%over a givenperiod oftime.
- Nebulization should be continued for about a minute afterthe'spluttering'*occurs.
*Spluttering:Change in the sound, indicating dryness in medication chamber.
Cleaning Of the Nebulizer
To prevent the possible risk of infection, cleaning of the nebulizer is recommended after each treatment.
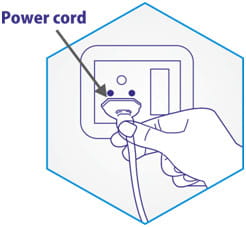
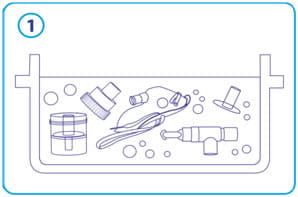
1. With the power switch off, unplug the power cord.

2. Disconnect the tubing from the air outlet.

3. Disassemble the mouthpiece or face mask from the cap. Open the medication cap and remove the baffle.
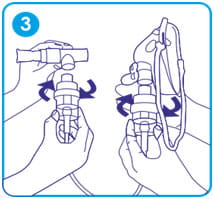
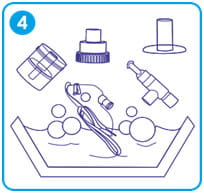
4. Wash all the accessories (except the tubing), in warm water/mild detergent solution. Rinse with warm water to remove detergent residue. Allow to air-dry.
5. Wipe the outer surface of the tubing regularly. If you notice some liquid droplets in the tubing, connect it to the compressor air outlet, switch on the compressor and blow air through the tubing for a few seconds.

Care and Maintenance of the Nebulizer
Disinfect daily
Step1
Using a clean container, soak all the accessories (except the tubing) for 30 minutes in
• Commercially available medical disinfectant or
• Mild detergent or
• Vinegar solution (1 part white vinegar and 3 parts warm water)
Step 2
With clean hands, rinse all the accessories with warm water, and air-dry.

Maintenance
- Do not open the compressor cabinet. All disassembly and maintenance must be done by the manufacturer.
- Filter- The filter should be changed when it discolours totally. Do not reuse or wash the filter or substitute it with any other material.

• Compressor- Wipe the outside of the compressor with a clean cloth regularly.

For more information, please refer the manufacturer’s user manual.
Key Aspects of Nebulization
|
IMPORTANT POINTS: NEBULIZATION THERAPY |
RATIONALE |
|
Ensure the type of medication and correct dosage needed for the patient |
To exclude contraindicated patients and for correct dilution |
|
Drug compatibility should be checked prior delivering drugs through a nebulizer |
For possible drug incompatibility and to ensure optimum fill volume |
|
Oxygen can be used as the driving gas, at 6-8 lit/min in patients with severe obstruction |
Oxygen may be required in patients with hypoxia. Monitoring patients during this treatment is required |
|
Assist patient into a comfortable position, preferably sitting upright and advice him/her to to take normal steady breaths (tidal breathing) and occasional deep breaths. |
To minimize dyspnoea and to allow maximum lung expansion in order to ensure medication reaches the bronchioles. |
|
Wash and dry hands before handling the nebulizer system |
To reduce the risk of cross infection |
|
A mouth piece should be preferred, when delivering steroids, anticholinergics and antibiotics |
This may reduce the risk of side effects |
|
A tight sealed mask can be used in acutely ill patients, babies, young children or who are unable to hold the mouthpiece |
Ill patients may get exhausted holding the mouthpiece. Drug delivery may be reduced, if the mask is loose fitted |
|
Keep the nebulizer chamber upright while in use |
This allows maximum amount of drug to be delivered effectively |
|
The fill volume should be 2-5 ml. |
For a nebulizer to work efficiently, correct fill volume should be ensured |
|
Occasional tapping of the medication chamber during nebulization |
This shakes down the large droplets to the chamber and ensures maximum delivery of the drug |
|
Nebulization should be ceased after 5-10 minutes |
Nebulizers should not be run to ‘dryness’, small amount of liquid will always remain in the medication chamber |
|
Ensure thatthe nebulizer accessories are washed, between doses, when administering more than one type of medication |
To prevent drug interactions |
|
Encourage the patient to rinse the mouth with water and spit out, after nebulization |
To reduce the risk of oral thrush and systemic side effects |
|
After each use, discard the remaining liquid |
To reduce the risk of colonization of the nebulization chamber |
|
Wash all the accessories (except tubing) with warm water/mild detergent, after each use |
Organisms may multiply in any fluid left in the nebulizer unit and may then be inhaled by the patient |
|
All the accessories (except tubing) should be disinfected regularly(at least once a day) |
To reduce the risk of colonization |
|
If there is condensation present in the tubing, reconnect the tubing to the compressor and allow air to blow through it |
Wet tubing may encourage the growth of bacteria.This process will remove excess water and drug crystals that may be present in the tubing |
|
The nebulizer unit should be covered and stored |
To keep it clean and dust free |
|
Compressor functioning should be checked and maintained regularly |
The compressor has to be efficient enough to deliver the drug and safe to use. |
References
- Ann EmergMed.2000;36:198-203
- Chest2007; 131:286-289
- Ann AllergyAsthmaImmunol.1998;80:499-508
- JAsthma1997;34(6):521-530
- CochraneDatabaseSystRev.2003;(4):CD001115
- J AerosolMed2007; 20(7): S78-84
- AmJRespirCritCareMed2000;162:593-598
- RespirCare2000;45(6):609-622
- J Asthma2002;39(4):337-339
- Thorax 1997;52(5uppl2): S1-S106
- EurRespirJ200 7;18:228-242
- User Manual of Nebuflo Compressor Nebulizer System: Jay PrecisionProducts
- http://www.nottingham.ac.uk/mhs/documents/c/inicalskills/nuh-guidelines/nebu/iser.pdf (Accessed on 27thMarch2014)