Introduction
Inhalation therapy is the cornerstone in the management of respiratory tract disorders such as asthma and COPD. Nowadays, a wide range of inhalers are available in the market, which help the physicians to individualize the treatment for their patients. Physicians play a very important role in management of these diseases by prescribing the right device for their patients and also by addressing other aspects such as counselling patients on the use of inhalers, demonstrating and teaching correct techniques and resolving patient queries. There are many myths associated with inhalation devices amongst patients which act as a barrier to their use and may lead to poor adherence to therapy. Poor adherence means increased risk of exacerbations and increased health-care costs.
Thus, it is imperative that physicians are well informed on the subject of inhalation devices and also are aware of the common barriers while prescribing inhaler devices.
Methods
A questionnaire-based survey to find out-
- Respiratory physicians’ knowledge
- Barriers faced while prescribing inhalation therapy
- Criteria for selection of inhalers
- Methodology adopted for training patients
Results
- 30% physicians felt confident about their knowledge and understanding of inhaler devices and 55% physicians said that they needed more information on the inhalation devices.
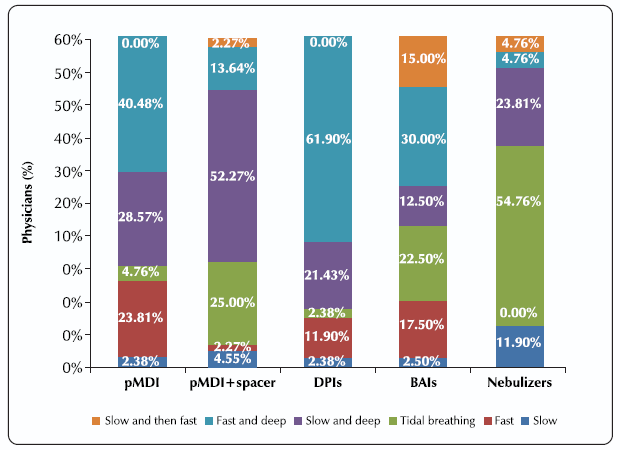
- Most physicians had queries regarding the correct breathing pattern required for different types of inhalers such as pMDIs, DPIs, BAIs and Nebulizers. It is crucial that each device is operated with its correct technique to achieve maximum benefits.
- 40% of the physicians were not sure whether the patients clean their inhalation devices. Maintaining hygiene in inhalation devices is of paramount importance. The goal of aerosol therapy is to medicate, not contaminate; hence its imperative that physicians stress about proper cleaning and maintenance of inhalation devices to their patients.
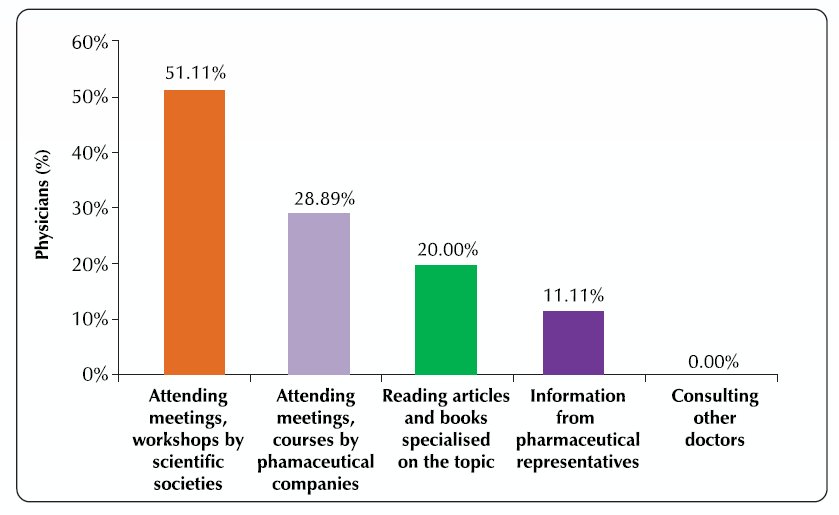
- Meetings, workshops and courses are the major source of knowledge for physicians on inhalation devices and specifically on the device technique.
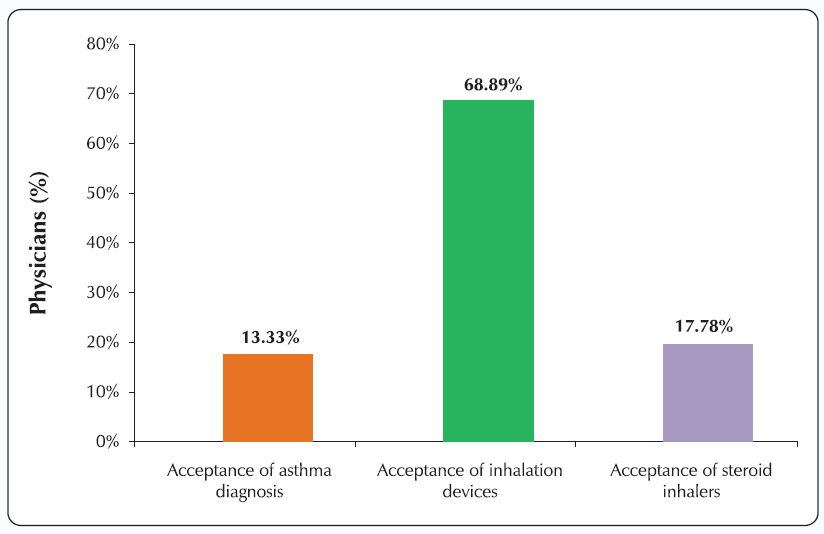
- Acceptance of inhalation devices by patients is the most important barrier faced by around 69% of the physicians. In India, particularly in rural areas, where asthma is still considered to be a taboo topic, many patients resist inhalation therapy due to social pressure also.
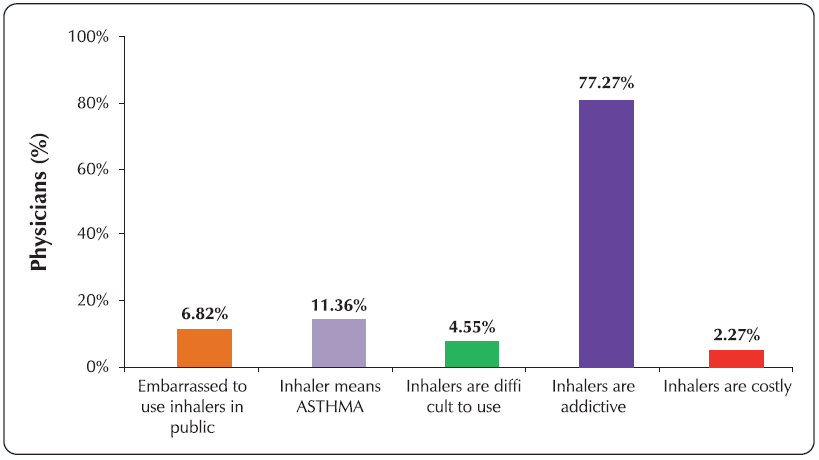
- 4 out of 5 physicians said that the most common reason for not accepting inhalers by patients is the notion that ‘inhalers are addictive’. It is such misconceptions that lead to poorer disease outcomes in patients. Educating the patients in correct use of inhalers and explain the importance of why inhalation therapy is superior will go a long way in correcting such misconceptions.
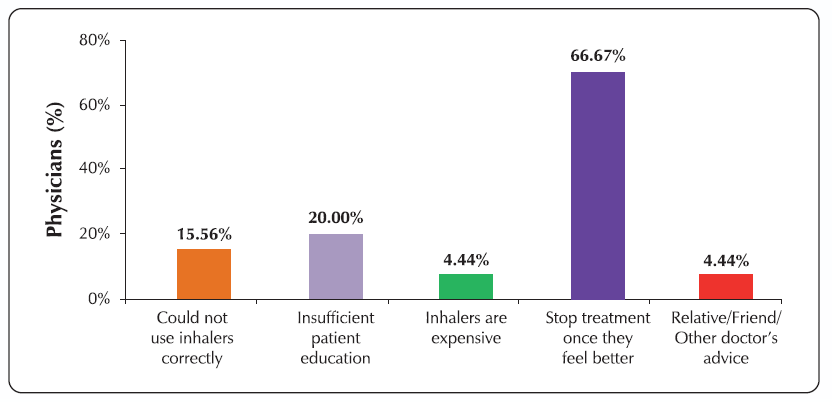
- 84% physicians said that more than 40% patients do not adhere to treatment and stop the use of inhalers once they feel better.
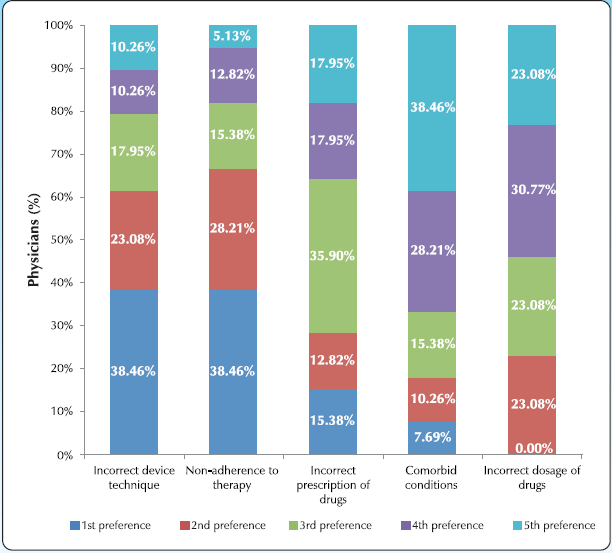
- More than 60% physicians feel that incorrect device technique and non-adherence to therapy are responsible for poor disease outcomes. With correct patient education, both these factors can be controlled, and this would help achieve better disease outcomes.
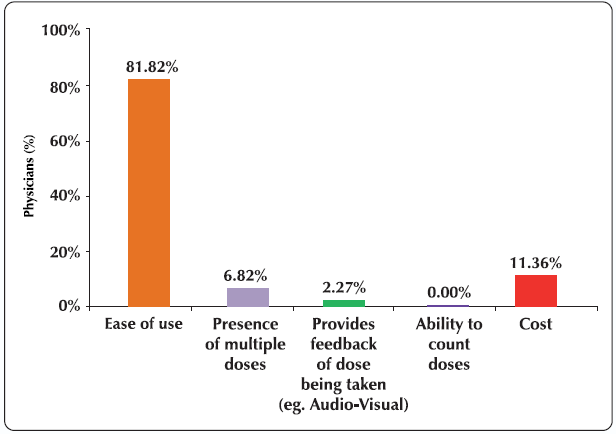
- Selection of inhaler device by physicians is based on ease of use, competence of patient and severity of disease. Devices must be easy to use for patients as it would help ensure adherence to prescribed therapy.
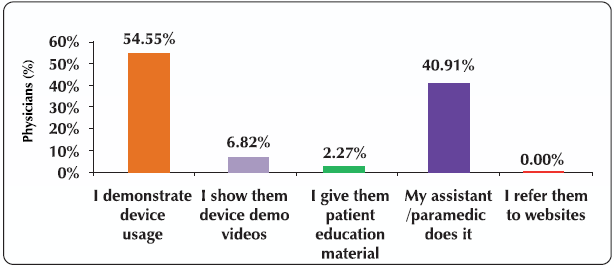
- 95% physicians felt that one-to-one live demonstration (by themselves or assistant paramedic) using placebo inhaler is the most effective way to teach the inhaler technique. There can be no doubt that physical demonstration with a placebo inhaler is the best way to teach correct inhalation technique.
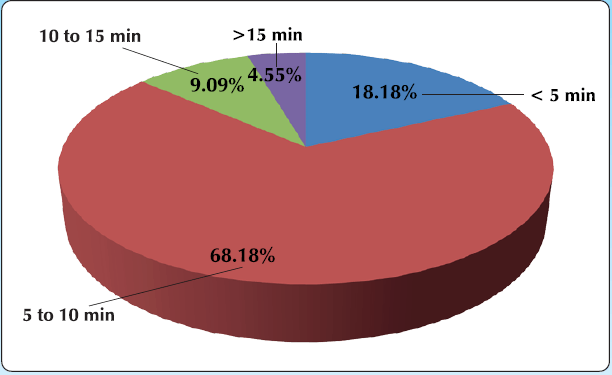
- 86% of physicians and paramedics spend less than 10 minutes for training patients on how to use their inhalers correctly, at the first visit. In the busy Indian clinical set-up, doctors cannot spend more time on a single patient. However, this can be addressed by having special educators/paramedics who can spend more time per patient and ensure that they learn the correct inhalation techniques.
- 40% physicians most often prescribe a unit dose DPI and feel that it requires least time to teach compared to other devices such as pMDI, BAI, multi-dose DPI, etc. Dry powder inhalers are often the easiest to use device among the available range of devices. However, it should be kept in mind that DPIs work correctly only when sufficient inspiratory flow is generated and not otherwise.
Conclusion
The study sheds light on the scenario of inhalation devices in India. Many physicians have limited knowledge on inhalation devices, and the main source of information for the physicians is attending various meetings, workshops and courses conducted by scientific societies and pharmaceutical companies. There is a widespread resistance to acceptance of inhalation therapy by patients and this acts as a significant barrier for the practicing physicians.
Educating patients on benefits of inhalation therapy and correct technique of usage by investing sufficient time would help increase acceptance, adherence and correct usage of inhalers, thereby achieving better disease control.
Poster presented at NAPCON, November 05-07, Jaipur India