Role of Cefepime Enmetazobactam in HAP
Key Takeaways:
- Hospital-acquired pneumonia (HAP) is associated with significant morbidity, mortality, and increased healthcare costs.
- Common pathogens causing HAPs in India include A. baumannii, Staphylococcus aureus, K. pneumoniae, and P. aeruginosa.
- Cefepime/enmetazobactam is a novel β-lactam–β-lactamase inhibitor combination with broad-spectrum antimicrobial activity against a range of ESBLs (extended-spectrum beta-lactamase) and/or AmpC (Ambler class C β-lactamases)-producing Enterobacteriaceae.
- The Central Drugs Standard Control Organization (CDSCO, India)[1], the European Medicines Agency (EMA), and the United Kingdom Medicines and Healthcare Products Regulatory Agency (UKMHRA)[2] approved the combination of cefepime/enmetazobactam in 2024 for the treatment of HAP including ventilator-associated pneumonia (VAP) in patients who are 18 years of age or older.
Hospital-acquired pneumonia (HAP) is becoming more complicated due to the rise in multi-drug resistance (MDR) pathogens.[3] For the empirical treatment of serious Gram-negative infections in settings where ESBL-producing Enterobacteriaceae is anticipated, cefepime/enmetazobactam may offer a unique carbapenem-sparing therapeutic consideration.[4]
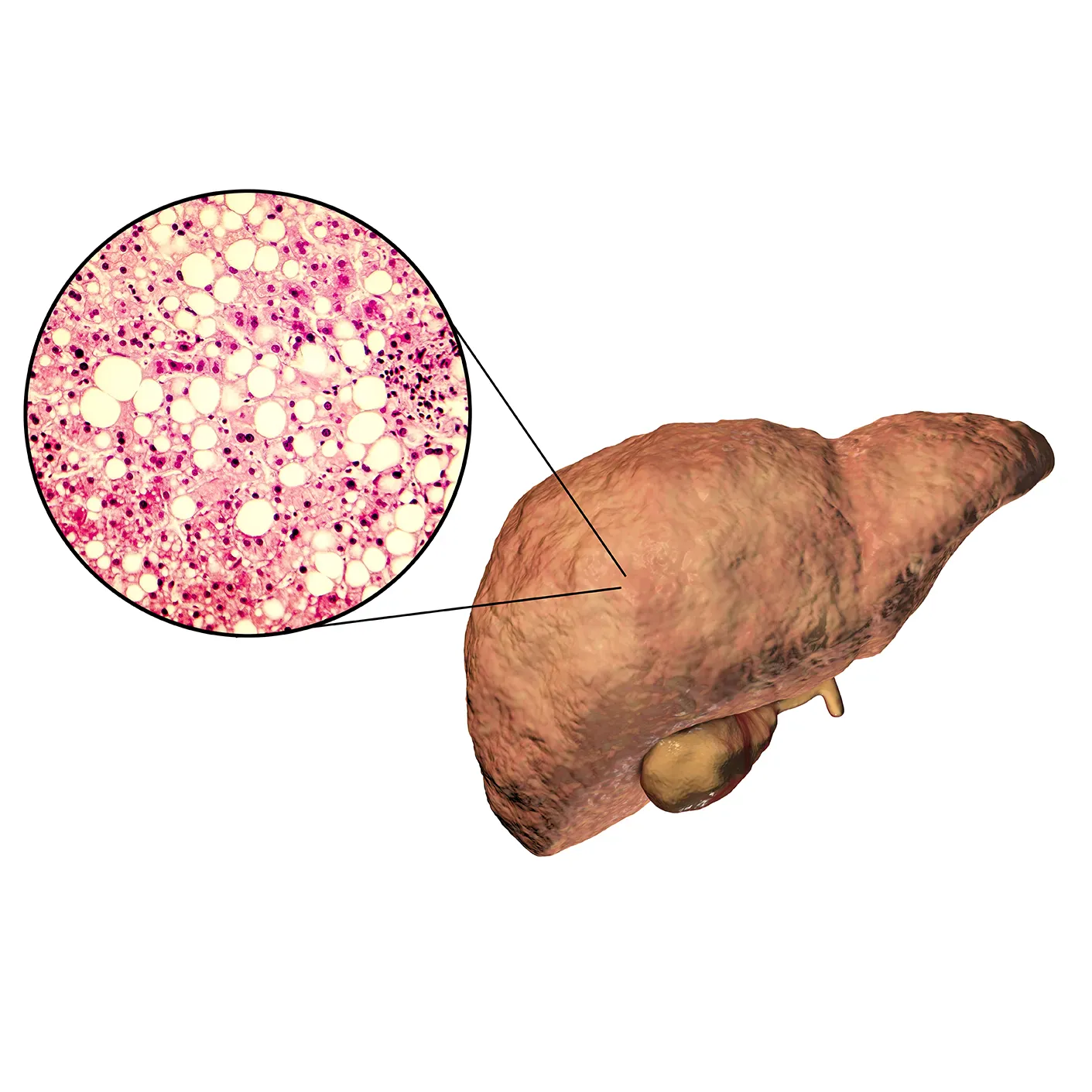
Indian Burden of Hospital Acquired Pneumonia:
HAP has been linked to attributed mortality rates of 33% to 50% and crude mortality rates of up to 70%. Ventilator-associated pneumonia (VAP), which is thought to be the most common infection in patients admitted to the intensive care unit (ICU), maybe the cause of death.[5] An Indian survey on the epidemiology of HAP in a tertiary care hospital revealed that the average HAP rate in India is 1.82 cases per 1000 admissions and is usually developed within an average of 11 ± 8 days.[6] Acinetobacter baumannii, Staphylococcus aureus, Klebsiella pneumoniae, and Pseudomonas aeruginosa are the most common pathogens causing HAPs in India.[7]
A randomised controlled study conducted across 263 hospitals in 34 countries, enrolling a total of 726 patients found that 31% of culture-positive nosocomial pneumonia patients were caused by ESBL-producing Enterobacteriaceae.[8] Cefepime/enmetazobactam is a novel β-lactam–β-lactamase inhibitor combination with broad-spectrum antimicrobial activity against a range of ESBLs and/or AmpC-producing Enterobacteriaceae. Enmetazobactam has potent activity against ESBLs, and cefepime is stable against hydrolysis by AmpC. Together, this combination has demonstrated potent activity against Enterobacteriaceae expressing ESBLs and/or AmpC.[9]
Cefepime/Enmetazobactam: Novel Treatment for Nosocomial Pneumonia:9
Das Shampa et.al, enrolled a total of 20 healthy volunteers to evaluate the intrapulmonary pharmacokinetics of a regimen of 2 g cefepime/1 g enmetazobactam every 8 h intravenously (2 g/1 g q8h i.v.). Each volunteer contributed multiple plasma samples and a single epithelial lining fluid (ELF) sample. The analysis of pharmacokinetic data showed that the concentration-time profiles of both agents in plasma and ELF were similar. The mean ± standard deviation percentage of partitioning total drug concentrations of cefepime and enmetazobactam between plasma and ELF was 60.59% ± 28.62% and 53.03% ± 21.05%, respectively. Using pharmacodynamic targets for cefepime of greater than the MIC (minimum inhibitory concentration) and free enmetazobactam concentrations of >2 mg/litre in ELF of 20% of the dosing interval, a regimen of cefepime/enmetazobactam of 2 g/0.5 g q8h i.v. infused over 2 h resulted in a probability of target attainment of ≥90% for Enterobacteriaceae with cefepime/enmetazobactam MICs of ≤8 mg/litre.
Figure 1: Correlation between area under the concentration-time curve in plasma and epithelial lining fluid (ELF) for cefepime and enmetazobactam, cefepime and enmetazobactam (A), ELF (B). Adapted from Das, Shampa et al. Antimicrobial Agents and Chemotherapy vol. 65,1 e01468-20. 16 Dec. 2020, doi:10.1128/AAC.01468-20
There was a strong correlation (r = 0.642, P < 0.01, n = 19) between the estimates of plasma exposure for cefepime and enmetazobactam, and an even stronger relationship (r = 0.916, P < 0.001, n = 19) for ELF, indicating that the two test items have similar pharmacokinetic properties (see figure 1). The pharmacodynamic rationale provided within this study supports the use of cefepime/enmetazobactam in the treatment of nosocomial pneumonia.
A combination of cefepime/enmetazobactam can be used to treat HAP/VAP caused by ESBL-producing Enterobacteriaceae and other Gram-negative pathogens.[1]DCGI Approval for antibiotic drug combination of cefepime and enmetazobactam. Retrieved on 15th July 2024 from https://www.expresspharma.in/orchid-pharma-receives-dcgi-approval-for-its-antibiotic-drug-combination-of-cefepime-and-enmetazobactam-nce/
[2]Keam SJ. Cefepime/Enmetazobactam: First Approval. Drugs. 2024 Jun;84(6):737-744. doi: 10.1007/s40265-024-02035-2. Epub 2024 May 18. PMID: 38761353.
[3] Bassetti, Matteo, and Javier Garau. “Current and future perspectives in the treatment of multidrug-resistant Gram-negative infections.” The Journal of antimicrobial chemotherapy vol. 76,Suppl 4 (2021): iv23-iv37. doi:10.1093/jac/dkab352
[4] Morrissey, Ian et al. “In Vitro Activity of Cefepime-Enmetazobactam against Gram-Negative Isolates Collected from U.S. and European Hospitals during 2014-2015.” Antimicrobial agents and chemotherapy vol. 63,7 e00514-19. 24 Jun. 2019, doi:10.1128/AAC.00514-19
[5] Chawla, Rajesh. “Epidemiology, etiology, and diagnosis of hospital-acquired pneumonia and ventilator-associated pneumonia in Asian countries.” American journal of infection control vol. 36,4 Suppl (2008): S93-100. doi:10.1016/j.ajic.2007.05.011
[6] Bhadade, Rakesh et al. “Emerging trends of nosocomial pneumonia in intensive care unit of a tertiary care public teaching hospital in Western India.” Annals of African medicine vol. 16,3 (2017): 107-113. doi:10.4103/aam.aam_7_17
[7] Anand M Buch, Dhaval V Parmar, et.al,. An Insight on Epidemiology of Hospital Acquired Pneumonia In A Reference Tertiary Care Hospital Of The Saurashtra Kutch Area. 2020. International Journal of Scientific Research.
[8] Kollef, Marin H et al. “Ceftolozane-tazobactam versus meropenem for treatment of nosocomial pneumonia (ASPECT-NP): a randomised, controlled, double-blind, phase 3, non-inferiority trial.” The Lancet. Infectious diseases vol. 19,12 (2019): 1299-1311. doi:10.1016/S1473-3099(19)30403-7
[9] Das, Shampa et al. “Intrapulmonary Pharmacokinetics of Cefepime and Enmetazobactam in Healthy Volunteers: Towards New Treatments for Nosocomial Pneumonia.” Antimicrobial agents and chemotherapy vol. 65,1 e01468-20. 16 Dec. 2020, doi:10.1128/AAC.01468-20