Selection of Inhaler Devices
Currently, no single inhaler satisfies the needs of all patients. When choosing an inhaler, a patient's competence in using it and preference for one over another are important factors.There are different types of devices available in the market which vary based upon their size, mechanism, cost and technique required for usage. Hence, it is very important for physicians to choose the device which will best suit the patient. Patients will be more compliant if they have confidence in their inhalers.
The selection of an inhaler device depends upon many factors such as the ease of use, availability, durability, cost, skills and age of patients, severity of disease and, last but not the least, patient preference.
The physician and patient should jointly decide the inhaler that the patient needs to use. According to the GINA 2014 guideline, if different inhaler devices options are available, patients should be encouraged to participate in the choice.
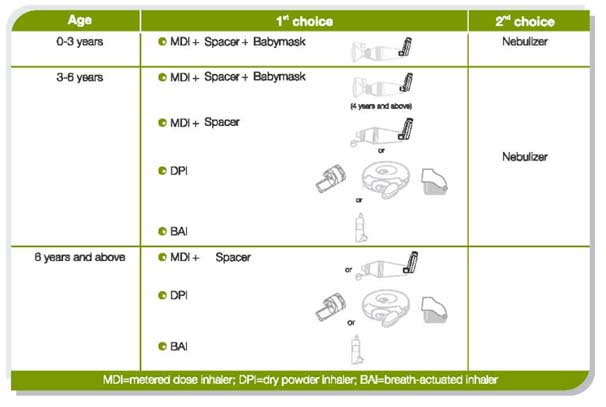
Table 1: Selection of devices according to the patient’s age
In case of very small children (age 0-4 years), a pMDI + spacer + face mask isthe most suitable device as the child can only inhale tidally and cannot hold a mouthpiece of spacer. Alternatively, nebulizers can be used.
Children above 4 years of age can hold a spacer and can be trained to inhale through the inhaler. Hence, a pMDI + spacer is an ideal device in this age group. Alternatively, a nebulizer can be used.
Older children (aged 6 years and above) can easily use a pMDI + spacer and a BAI (autohaler). If they can produce sufficient inhalation effort, dry powder inhalers (Rotahaler, Revolizer etc) can also be prescribed.
Adults can use all the devices; the selection in this case should also take into account the preference of the patient.
Elderly patients have co-ordination and visual problem. Hence, for them, either pMDI + spacer, BAI (autohaler) or a Nebulizer should be preferred. They can also use other devices depending upon their condition and preference.
The ideal device is the one that suits the patient the best. Overall, all the inhaler devices are similar as long as the technique of using the particular device is correct.
Selection of a Device during Exacerbations/Attacks
The selection of a device during asthma and COPD exacerbation depends upon the severity of the attack, ease of use and also how quickly the medication can be taken through the device.
Nebulizers are the most convenient during an emergency situation. Studies have shown that a pMDI+spacer is an equally effective as a nebulizer. Several studies have demonstrated similar efficacy for inhaled bronchodilators using pMDIs + spacers, compared with nebulizers, in emergency rooms in asthma and COPD patients.
Breath actuated inhalers (Autohaler) is also a good choice during attacks as it is very easy to use, requires very less inhalation effort and does not require actuation and inhalation co-ordination.
DPIs are not a very good choice during an exacerbation as patients need to generate a high inspiratory flow rate to inhale through the device. However, a few patients could manage to generate the inspiratory flow required to activate the DPIs during asthma attacks.
Selection of Device in COPD Patients
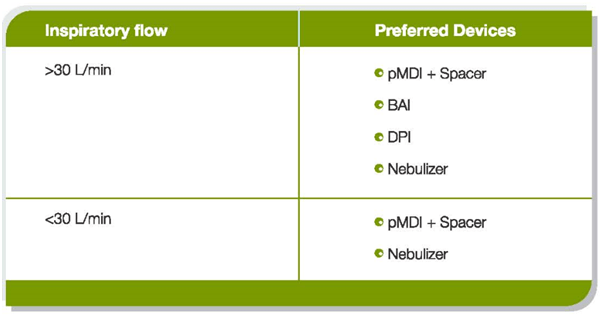
The severe expiratory airflow limitation in COPD is typically accompanied by decreasedinspiratory capacity, hyperinflation and respiratory muscles that work at a mechanical disadvantage. All of these factors combine to reduce inspiratory flow rates. The inspiratory flow rate also reduces as the person ages and a reduce inspiratory flow rate is associated with poor lung deposition.
DPIs and BAIs can be selected for those COPD patients who can generate an inspiratory flow of more than 30L/min.
Further, in older COPD patients, cognitive function and manual dexterity is impaired while hand strength and inspiratory capacity is reduced. These factors should also be taken into consideration before selecting an inhaler device for a COPD patient.
COPD patients with sufficient inspiratory capacity and good manual dexterity and strength can use pMDIs as well as DPIs. DPIs should be preferred in these patients as studies have shown that patients make fewer device handling mistakes with a DPI than a pMDI or pMDI+spacer.
Patients with mild-to-moderate impairment of manual dexterity may have difficulty with the hand–breath coordination required to use a pMDI, to generate the minimum force required to activate a pMDI device, and also for dosage preparations (loading, puncturing and disposing) with single-dose DPIs. Further, these patients may also find it difficult to raise and lower the lever of an Autohaler.
Nebulizers should be preferred in those COPD patients who cannot hold their breath for more than 5 seconds. Further, it can also be used in COPD patients, who cannot use a pMDI or DPI correctly despite appropriate instruction and demonstration due to locomotor, visual or cognitive limitations. Patients might require a care-giver or family member or relative to assist with the preparation and maintenance of a nebulizer.
Further, COPD patients suffer from many comorbidities and age-related illness and, therefore, may be taking multiple medications. According to a study, at any point in time, elderly patients with COPD may be receiving an average of 6.2 prescription medications. This is a substantial cost for the patient. So care should be taken to prescribe devices and medication that are not very expensive.
Prescribing Multiple Inhalers to the Same Patient
The medicines for treating asthma and COPD are available in different devices such as pMDIs, DPIs, Respules etc. Many doctors tend to prescribe different devices to the same patients, i.e. they prescribe two different devices for reliever and controller. It must be noted that patients often find it difficult to learn and remember the usage techniques for different inhalers.
A study have shown that use of more than one type of inhaler increased the likelihood (odds ratio= 2.92) of incorrect handling of either inhaler.Use of devices such as the pMDI and DPI in combination may increase the potential for inhaler misuse. Further, another study showed that the percentage of patients performing all the steps correctly was greater when a combination of DPIs was used, compared to a combination of a pMDI and DPI.
Choosing the same type of device for treatment of acute and chronic symptoms may facilitate teaching and reduce the potential for confusion and error.
Checklist – Questions To Be Kept In Mind before Selecting Inhaler Devices for Patients
- In what device is the drug(s) available?
- Which device would be easy to use for the patient depending on his or her age and clinical setting?
- Which devices are the least costly?
- Can the same device be used for delivering multiple drugs?
- Which devices are most convenient to the patient, family or medical staff taking into consideration the time required for drug administration, cleaning and portability of the device?
- How durable is the device?
- Does the patient or clinician have any specific device preferences?
Tips for Selecting the Most Appropriate Device
- Consider the patient’s age, skill, disease severity and inhaler ease of use, availability, durability and cost before selecting any device for the patient.
- The physician and the patient should jointly decide the inhaler for the patient. Patients should be encouraged to participate in the choice.
- A pMDI + spacer + face mask is the most suitable device in small children (age 0-4 years); a nebulizer can also be used. A pMDI + spacer is an ideal device in children aged above 4 years as they can hold a spacer and can be trained to inhale through the inhaler. Alternatively, a nebulizer can be also used.
- Nebulizers are the most convenient during an emergency situation. Studies have shown that a pMDI+spacer is as equally effective as a nebulizer.
- In older COPD patients, cognitive function and manual dexterity is impaired while hand strength and inspiratory capacity is reduced. These factors should be taken into consideration before selecting an inhaler device for a COPD patient.
- DPIs and BAIs should not be prescribed to those COPD patients who cannot generate sufficient inspiratory flow effort (>30 L/min).
- Choose the same type of device for the treatment of acute and chronic symptoms.
- An inhaler with a dose counter should be preferred.
- Consult the family or care-givers before prescribing the device.
- Physicians should train patients on using the device correctly at every clinic visit. Ensure that the patient is using the device correctly.
- The ideal device is the one that suits the patient the best.
- All the inhaler devices are similar as long as the technique of using the particular device is correct.
References
- Global Initiative For Asthma (GINA), 2015
- Am J Health-Syst Pharm. 2011; 68:1221-32
- Eur Respir J 2011; 37: 1308–1331
- Chest 2002; 121: 1036–1041
- Eur Respir Rev 2005; 14(96) : 117–122
- Prim Care Resp J 2010; 19(1): 10-20