Alternative Antithrombotic Pathways In Acute Myocardial Infarction With Large Thrombus Burden: A Randomized Trial ARISE-ARMYDA 7
Speaker: Dr. Marco G. Mennuni
Key Highlights
Introduction:
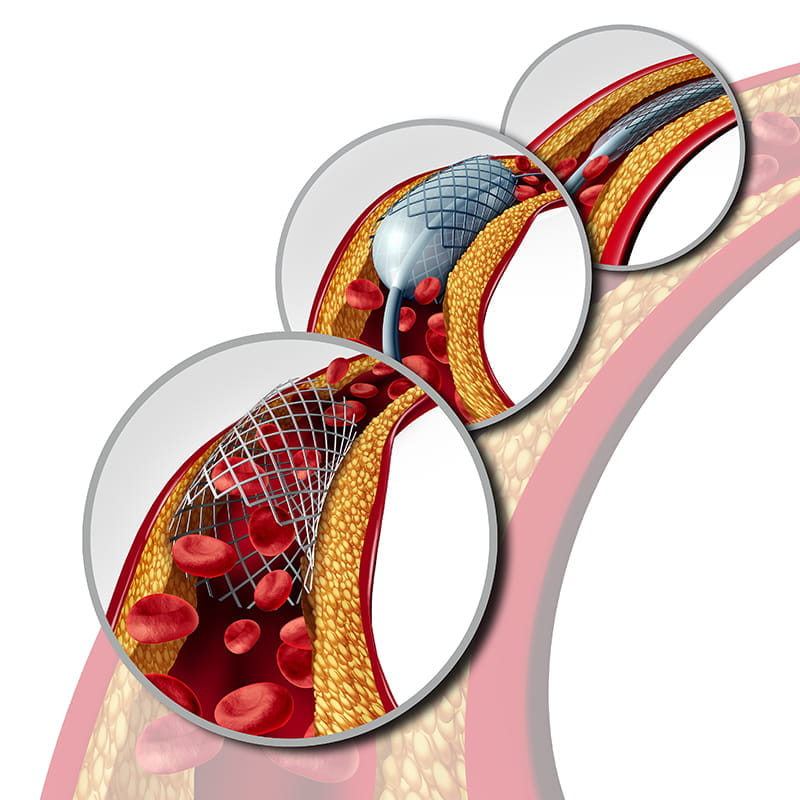
Findings from the ARISE-ARMYDA 7 trial, a mechanistic pilot study exploring an alternative antithrombotic approach in STEMI patients with large intracoronary thrombus burden were presented. The trial assessed whether short-term use of low-dose Rivaroxaban added to DAPT could reduce thrombus burden without increasing bleeding risk.
Aim:
To assess if Rivaroxaban 2.5 mg BID added to DAPT for 5–7 days can enhance thrombus resolution in STEMI patients with substantial thrombus burden, without increasing bleeding risk.
Method:
-
Design: Randomized, open-label, mechanistic pilot study
-
Participants: 44 low-risk STEMI patients with large thrombus confirmed angiographically
-
Intervention:
-
Intervention group: DAPT + Rivaroxaban (2.5 mg BID) for 5–7 days
-
Control group: DAPT alone
-
Primary endpoint: Reduction in thrombus burden as measured by OCT-derived thrombus score
-
Secondary endpoints:
-
OCT-based thrombus metrics: volume, length, area
-
30-day MACE
-
Bleeding events (BARC classification)
Results:
-
Primary Outcome – Thrombus Score Reduction:
-
Rivaroxaban group: 60% reduction
-
Control group: 36% reduction
-
Absolute thrombus score change: −66 quadrants (Rivaroxaban) vs. −44 quadrants (control)
-
Statistically significant superiority in the Rivaroxaban group
-
Secondary OCT Metrics:
-
Greater reductions in thrombus volume, area, and length observed in the Rivaroxaban group, supporting the primary endpoint findings.
-
Bleeding Events:
-
No major bleeding in either group
-
Minor bleeding occurred in only 2 patients in the Rivaroxaban arm
-
Overall, Rivaroxaban demonstrated a favourable safety profile
-
MACE at 30 Days:
-
Only one myocardial infarction occurred (group not specified)
-
No deaths, strokes, or target vessel revascularizations reported
-
Event rates were very low across both groups
Conclusion:
The ARISE-ARMYDA 7 trial showed that short-term, early use of low-dose rivaroxaban with DAPT significantly reduced thrombus burden in STEMI patients with large thrombi, without increasing major bleeding. These pilot results highlight a promising dual-pathway inhibition strategy and justify further investigation in larger clinical trials.
Efficacy and Safety of Azd0780, an Oral Small Molecule Pcsk9 Inhibitor for Treatment of Hypercholesterolemia: Results from a Ph2b Randomized Placebo-Controlled Clinical Trial
Speaker: Dr. Michael J. Koren
Key Highlights
Introduction:
A novel oral PCSK9 inhibitor, AZD0780, was evaluated in patients with hypercholesterolemia inadequately controlled on moderate to high-intensity statins. A distinct mechanism was employed by AZD0780—binding to the C-terminal domain of PCSK9 to prevent lysosomal degradation of LDL receptors, thereby enhancing their recycling. Oral administration was allowed without food restrictions.
Methods:
-
Conducted as a randomized, placebo-controlled, global Phase 2b trial at 55 sites across 8 countries.
-
A total of 426 adults with LDL-C between 70–109 mg/dL on background statins were enrolled.
-
Patients were randomized to four AZD0780 doses or placebo.
-
The primary endpoint was defined as percent change in LDL-C at 12 weeks.
Results:
-
Efficacy Findings:
-
LDL-C Reduction:
-
A dose-dependent LDL-C reduction was observed.
-
At 30 mg daily, a 50.7% placebo-adjusted LDL-C reduction was achieved by week 12.
-
The effect was seen to plateau by week 2 and was maintained through week 12.
-
Secondary Lipid Parameters:
-
Total cholesterol was reduced by 29.4%.
-
Non-HDL-C decreased by 45.2%.
-
ApoB was lowered by 40% & Lp(a) showed a reduction of 19.5% at the 30 mg dose.
-
LDL-C Goal Attainment:
-
In post hoc analysis, 84.2% of patients in the 30 mg group met the ACC/AHA target of <70 mg/dL.
-
In contrast, only 13% of placebo patients achieved the same goal.
-
Safety and Tolerability
-
AZD0780 was reported to be well tolerated.
-
Adverse events occurred in 38.2% of AZD0780-treated patients vs. 32.6% in placebo.
-
Serious adverse events occurred in 2.1% but were not attributed to the drug.
-
Discontinuation due to AEs was low: 1.5% with AZD0780 vs. 2.3% with placebo.
Conclusion:
AZD0780 demonstrated potent LDL-C lowering, favorable safety, and strong treatment adherence potential. The once-daily oral formulation was highlighted as a potential advantage for adherence and overcoming treatment inertia. The PURSUIT trial findings suggest that AZD0780 could offer a convenient, effective oral alternative in lipid management—pending validation in outcomes-based studies.
Effectiveness of The 0/1-hour Algorithm for Chest Pain Assessment in Patients Presenting to the Emergency Department: A Multicenter Study in Asian Countries
Speaker: Dr. Kenji Inoue
Key Highlights
Introduction:
The effectiveness and safety of the 0/1-hour high-sensitivity troponin algorithm were evaluated in a multicentre, stepped-wedge cluster randomized controlled trial across emergency departments (EDs) in Asia. The study was conducted to address variability in guideline adoption and assay use across the region. High NSTEMI mortality in Southeast Asia (6–12%) was attributed to inconsistent use of protocols, in contrast to lower rates in Japan (2%). The algorithm, recommended by the European Society of Cardiology (ESC), was assessed against usual care for chest pain evaluation.
Methods:
-
Study Setting: The study was conducted across emergency departments in several Asian countries, including Japan, Malaysia, Taiwan, and others.
-
Population: Adult patients presenting to the ED with chest pain suspected to be of cardiac origin were enrolled.
-
Design: The stepped-wedge design meant that all participating centers eventually implemented the 0/1-hour algorithm, but in a staggered, randomized order:
-
Each site initially continued usual care.
-
A 1.5-month transition and training period was then used to familiarize clinicians with the algorithm and ensure operational readiness.
-
Sites then transitioned to using the algorithm.
-
Algorithm Implementation:
-
Patients were assessed using high-sensitivity cardiac troponin (hs-cTn) levels at baseline (0 hour) and 1 hour.
-
Based on predefined cutoff levels, patients were categorized into rule-in, rule-out, or observe groups.
-
Primary Endpoint: 30-day Major Adverse Cardiac Events (MACE), including myocardial infarction (MI), death, and urgent revascularization.
-
Secondary Endpoints: ED length of stay, physician adherence to algorithm recommendations, and operational efficiency metrics.
Results:
-
MACE and Risk Stratification
-
A 1.4% MACE rate was reported in the algorithm group, versus 1.7% with usual care, confirming non-inferiority.
-
No myocardial infarctions (MI) were reported among patients ruled out by the algorithm.
-
Among patients ruled in, 50% were confirmed to have MI.
-
Physician Adherence and Missed Diagnoses
-
The algorithm's rule-out results were followed in 75% of cases, enabling discharge of 85% of patients within 4 hours.
-
In 19% of rule-in cases, non-adherence led to 8 missed MIs.
-
Length of Stay and Operational Impact: The average ED stay was reduced to 160 minutes, confirming time-saving benefits previously noted in European trials.
-
System-Level Observations
-
Implementation challenges due to ED congestion and resource constraints were observed, especially in Malaysia and Taiwan.
-
Assay sensitivity differences and cost barriers were identified as limiting factors for algorithm uptake.
Conclusion:
-
The 0/1-hour algorithm was found to be safe and effective for use across Asian EDs.
-
It enabled faster, accurate rule-out of MI without increased adverse outcomes.
-
Consistency in performance was maintained across varying troponin assay thresholds.
-
A 70% healthcare cost reduction was preliminarily reported in Japan when using the algorithm.
-
Emphasis was placed on the need for local adaptations, including point-of-care testing, cost-effectiveness studies, and regional guidelines.
ACC.25, March 29 - 31, 2025, Chicago