Oral Semaglutide Reduces Cardiovascular Events In People With Type 2 Diabetes With Atherosclerotic Cardiovascular And/or Chronic Kidney Disease: Primary Results From The SOUL Randomized Trial
Speaker: Dr. Darren K. McGuire
Key Highlights
Introduction:
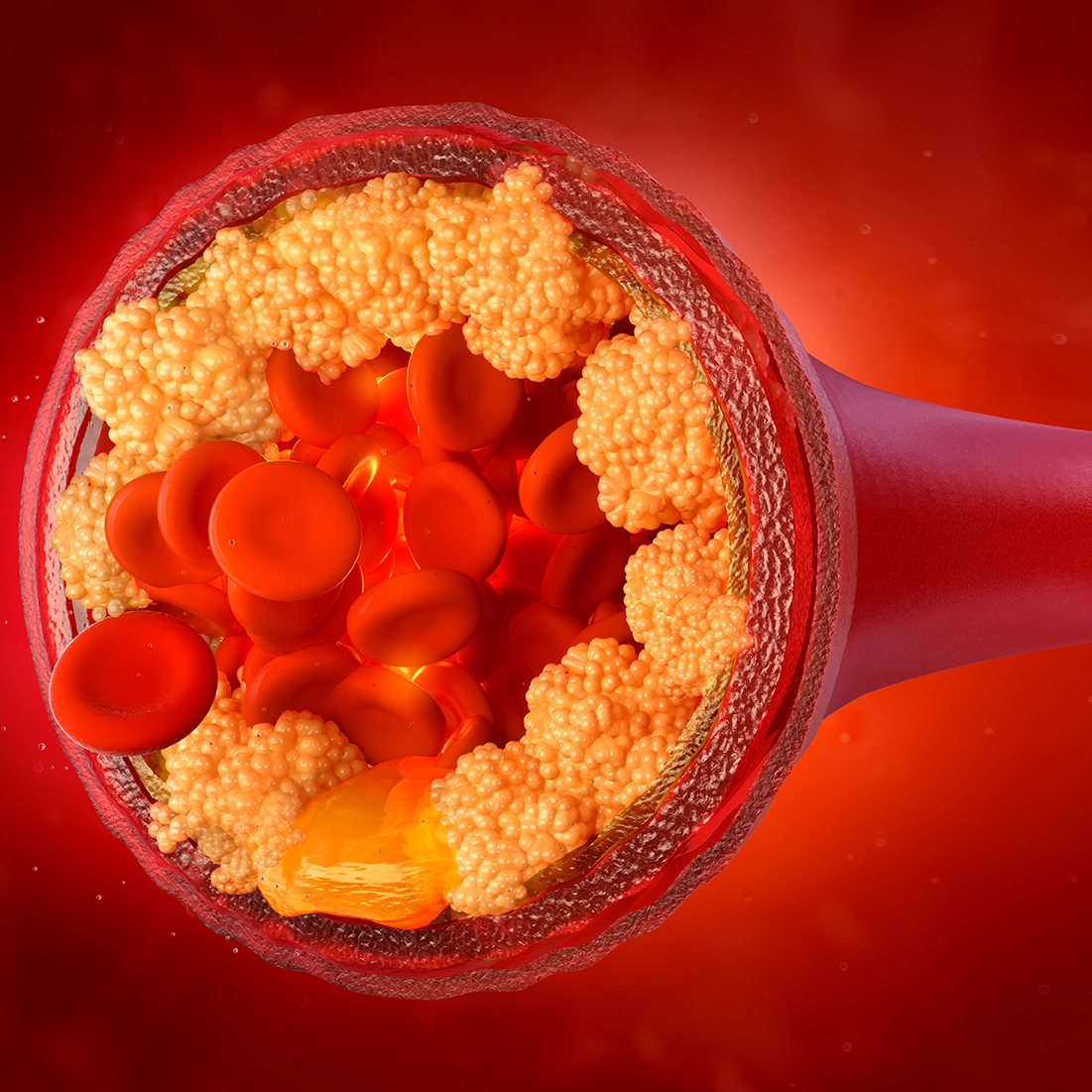
Semaglutide, a GLP-1 receptor agonist, has been widely studied for its efficacy in managing type 2 diabetes (T2D) and its potential cardiovascular (CV) benefits. The latest trial evaluated the impact of oral semaglutide on major adverse cardiovascular events (MACE) in patients with T2D and established atherosclerotic cardiovascular disease (ASCVD) or chronic kidney disease (CKD). The study also assessed its safety profile and consistency of benefits across subgroups.
Study Overview:
-
Study Design: Randomized, double-blind, placebo-controlled trial.
-
Population: Patients with T2D and either ASCVD or CKD.
-
Sample Size: 9,650 participants.
-
Inclusion Criteria:
-
Diagnosed T2D.
-
Established ASCVD (prior MI, stroke, or symptomatic peripheral artery disease) or CKD (eGFR 15-59 mL/min/1.73m²).
-
Exclusion Criteria:
-
Severe heart failure (NYHA Class IV).
-
Recent CV events within 60 days.
-
Prior GLP-1 receptor agonist use within 30 days before screening.
-
Intervention: Participants were assigned to receive oral semaglutide (14 mg once daily) or placebo, in addition to standard-of-care therapy.
-
Primary Endpoint: Time to first occurrence of 3-point MACE (CV death, non-fatal myocardial infarction, or non-fatal stroke).
-
Secondary Endpoints: Kidney outcomes and major adverse limb events.
-
Subgroup Analyses: Evaluated the consistency of effects across sex, age, BMI, HbA1c, eGFR, and background SGLT2 inhibitor use.
Baseline Characteristics:
-
Mean age: 66 years, 70% male
-
Mean HbA1c: 8.0%, Mean BMI: 31
-
Mean diabetes duration: 15 years (advanced disease)
-
Mean eGFR: 74 mL/min/1.73m² (preserved kidney function)
-
SGLT2 inhibitor use: 25% at baseline, 50% at some point during the trial
Results:
-
Primary Outcome: 3-Point MACE (CV Death, MI, Stroke)
-
Semaglutide group showed a 14% relative risk reduction (HR: 0.86, p=0.0028)
-
Curves diverged within 6 months and continued to separate over time
-
Absolute risk reduction: 2% at 3 years (NNT: 50)
-
Secondary Outcomes:
-
5-Point Kidney Composite Outcome: HR: 0.91 (p=0.0967, not statistically significant)
-
CV Death: HR: 0.93 (not statistically significant)
-
Major Adverse Limb Events: HR: 0.71 (29% risk reduction, exploratory finding)
-
Directionally consistent benefits across other CV and renal endpoints
-
Subgroup analysis showed consistent effects across sex, age, BMI, HbA1c, eGFR, and background SGLT2 inhibitor use
Conclusion:
Oral semaglutide was superior to placebo in reducing 3-point MACE in patients with T2D and ASCVD/CKD. CV efficacy was consistent across key subgroups, including those on SGLT2 inhibitors. Safety profile aligned with previous semaglutide trials, with no new safety concerns. These findings reinforce the favorable benefit-risk profile of oral semaglutide in this population. Oral semaglutide is the first and only oral GLP-1 receptor agonist with proven cardiovascular benefits.
Dapagliflozin In Patients Undergoing Transcatheter Aortic Valve Implantantion
Speaker: Dr. Sergio Raposeiras Roubin
Key Highlights
Aortic Stenosis and its Management:
Aortic stenosis is one of the most common valvular heart diseases in Western countries, with an increasing prevalence due to population aging. While transcatheter aortic valve implantation (TAVI) has changed the management of aortic stenosis, patients still face high rates of heart failure (HF), particularly in the first year following TAVI.
Role of SGLT2 Inhibitors in Heart Failure:
SGLT2 inhibitors have demonstrated efficacy in reducing heart failure across all patient spectrums with HF. As a result, both European and American guidelines recommend their use in all patients with HF. However, clinical trials on SGLT2 inhibitors have largely excluded patients with HF secondary to valvular heart disease or those undergoing valvular interventions. Additionally, patients undergoing TAVI tend to be older, and those above 80 years of age are underrepresented in clinical trials.
The DAPA-TAVI Trial: Study Design:
Given this background, the DAPA-TAVI trial was conducted to evaluate the efficacy and safety of SGLT2 inhibitors in TAVI patients and elderly populations. This was a pragmatic, prospective, randomized, open-label, endpoint-driven clinical trial in which patients were assigned to receive or not receive dapagliflozin following TAVI.
Inclusion and Exclusion Criteria:
-
Inclusion Criteria:
-
Patients with severe aortic stenosis undergoing TAVI
-
Prior HF hospitalization
-
One or more of the following: left ventricular ejection fraction (LVEF) <40%, diabetes, or moderate renal dysfunction
-
Exclusion Criteria:
-
Contraindication for SGLT2 inhibitors
-
Major hypotension
-
Moderate renal dysfunction
-
Chronic urinary tract infection
Primary and Secondary Endpoints:
-
Primary Endpoint: Composite of all-cause mortality or worsening HF, defined as any HF hospitalization or urgent HF visit requiring intravenous diuretics.
-
Secondary Endpoints: Components of the primary endpoint, cardiovascular death, and the composite of cardiovascular death and HF hospitalization.
Study Population and Follow-up: The study enrolled 1,257 patients across 39 centers in Spain between January 2021 and December 2023. Final analysis included 605 patients in the dapagliflozin arm and 617 in the control arm. Median time from TAVI to randomization was 2 days. Crossover rate was 17% in the dapagliflozin group, 7% in the control group.
Baseline Characteristics:
-
Mean age: 82 years (range 60-99 years)
-
Nearly 50% of patients were women
-
43% had diabetes
-
17% had systolic dysfunction
-
Most had some degree of renal dysfunction
Results:
-
Primary endpoint (all-cause mortality or worsening HF):
-
Occurred in 124 patients (control group) vs. 91 patients (dapagliflozin group)
-
Significant hazard ratio: 0.72
-
Per-protocol analysis: hazard ratio 0.67
-
Consistent effect across subgroups (diabetes, systolic dysfunction, renal dysfunction)
-
Component analysis:
-
No difference in all-cause death
-
37% reduction in worsening HF with dapagliflozin
-
Benefit seen in both HF hospitalization and urgent HF visits
-
No difference in cardiovascular death, but significant benefit in composite of cardiovascular death or HF hospitalization.
-
Safety Outcomes:
-
Increased risk of genital infections and symptomatic hypotension in the dapagliflozin group.
-
No significant difference in other adverse events between the groups
Conclusion:
Among elderly patients with aortic stenosis undergoing TAVI at high risk of heart failure, dapagliflozin was safe and reduced the incidence of all-cause death and worsening heart failure.
ACC.25, March 29 - 31, 2025, Chicago