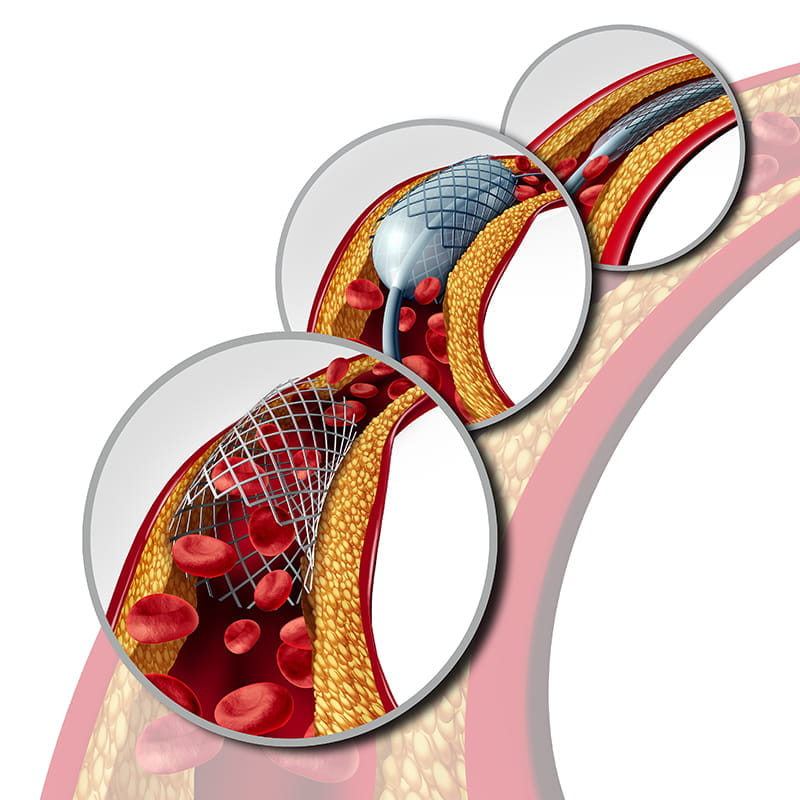
Fractional Flow Reserve Guided Percutaneous Coronary Intervention Compared with Bypass Surgery: Final 5 Year Results of the Fractional Flow Reserve Versus Angiography for Multivessel Evaluation 3 Trial
Speaker: Dr. William F. Fearon
Key Highlights
Introduction:
According to research on patients with 3-vessel coronary artery disease (3V-CAD), coronary artery bypass grafting (CABG) is less likely than percutaneous coronary intervention (PCI) to cause death, stroke, or myocardial infarction (MI) at long-term follow-up. These outcomes are dated given recent innovations in percutaneous and surgical techniques, and in medical therapy.
Aim:
The aim of Fractional Flow Reserve Vs Angiography for Multi-Vessel Evaluation (FAME) 3 trial was to compare fractional flow reserve (FFR)-guided PCI by using current-generation drug-eluting stent (DES) with contemporary CABG both used in conjunction with guideline-directed medical therapy. The objective of the study was to report the pre-specified final five-year follow-up of the FAME three trial.
Methods:
-
It was an investigator initiated, multicentre, randomized, controlled study.
-
The study included 1,500 participants, and they were divided into 2 groups:
-
Group 1- 742 people underwent PCI
-
Group 2- 690 people underwent CABG
-
Inclusion Criteria of the study was as follows:
-
The patient with 3V-CAD and 50% or more diameter stenosis in 3 major epicardial vessels (no left main involvement).
-
Should be amenable to both PCI and CABG
-
Exclusion criteria included the following:
-
Patients with Cardiogenic Shock
-
Patients who had STEMI within 5 days
-
Patients with LV ejection fraction of less than 30%
-
The primary end point of the study was to report the 5-year incidence of Death/Stroke/MI
Results:
The summary of the results is given below in the table:
|
Outcome |
PCI |
CABG |
Comments |
|
Primary Endpoint (Death, Stroke, or MI) |
16.00% |
14.10% |
Not statistically significant (HR 1.16; 95% CI 0.89–1.52; p=0.27) |
|
Death |
7.20% |
7.20% |
Identical in both groups |
|
Stroke |
Lower by 1.1% |
– |
Stroke occurred less commonly after PCI |
|
Myocardial Infarction (MI) |
Higher by 2.9% |
– |
MI more frequent in PCI group |
|
Repeat Revascularization |
Higher |
Lower |
More common after PCI |
|
Composite: Death, Stroke, MI, or Revascularization |
Higher |
Lower |
Worse in PCI group |
|
Alternative MI Definition (SCAI) |
20% |
23% |
Composite of Death, Stroke, or MI using SCAI criteria |
Death, MI or Stroke based on SYNTAX score:
-
Low SYNTAX score (<23): Patients showed better outcomes with PCI and compared to CABG. (95% CI 0.42-1.24)
-
Intermediate SYNTAX score (23-32): Patients showed better outcomes with CABG as compared to PCI. (95% CI 1.11-2.43)
-
High SYNTAX score (>32): No major difference between the two groups. (95% CI 0.43-1.60)
Conclusion:
In patients with 3V-CAD there was no significant difference in the composite of death, stroke, or MI after FFR guided PCI with a current DES in comparison with CABG after 5 years. This might be due to improved stent technology, routine application of FFR-guided PCI and greater adherence to guideline-directed medical therapy.
Clopidogrel Versus Aspirin for Long-term Maintenance Monotherapy in Patients with High Ischemic Risk after Percutaneous Coronary Intervention
Speaker- Dr. Joo-Yong Hahn
Key Highlights
Introduction:
Aspirin monotherapy following Dual Antiplatelet Therapy (DAPT) has been recommended as the standard practice for patients undergoing PCI in order to prevent subsequent events. However, there has been debate regarding the data that supports use of aspirin as a single antiplatelet after DAPT. Though there is limited evidence, Clopidogrel has been suggested as a superior alternative to aspirin.
Aim:
In patients who were at high risk of recurrent ischaemic episodes, the Smart Choice Trial sought to determine the safety and effectiveness of clopidogrel monotherapy in comparison to aspirin monotherapy after the usual DAPT period following PCI.
Methods:
-
SMART-CHOICE 3 was an investigator-initiated, randomized, open-labelled, multicentre trial which included 5506 patients who were at a high risk of Recurrent Ischemic Events and had completed a standard duration of DAPT after PCI.
-
The patients were divided into 2 groups:
-
Group 1: 2752 patients were assigned to the clopidogrel monotherapy group
-
Group 2: 2722 patients were assigned to the aspirin monotherapy group.
-
The inclusion criteria were as follows:
-
Patients aged 19 years or more who had undergone successful PCI with DESs and had received a standard duration of DAPT.
-
Patients who had at least one clinical characteristic (previous MI or medication-treated diabetes) or complex coronary artery lesion characteristic and had no vascular events after the index PCI.
-
The exclusion criteria were as follows:
-
Patients who were on ongoing treatment with oral anticoagulants and who were in a need for DAPT for any reason other than coronary artery disease.
-
Patients who had contradictions for usage of aspirin or clopidogrel.
-
Pregnant or breast feeding patient.
-
Patients with any non-cardiac co-morbid conditions with a life expectancy of 2 years.
-
Primary outcome: Major adverse cardiac and cerebrovascular events (MACCE), defined as a composite of:
-
Death from any cause
-
Myocardial infarction (MI)
-
Stroke
-
Secondary outcomes included:
-
Definite or probable stent thrombosis
-
Bleeding events
-
Upper gastrointestinal clinical events
-
Any revascularisation
Results:
The following results were recorded with a follow-up rate of 3 years for primary outcomes and 2.3 years for the secondary outcomes.
|
Outcome |
Aspirin Monotherapy |
Clopidogrel Monotherapy |
Measures |
|
MACCE |
6.6% |
4.4% |
CI 0.54-0.93; p=0.013 |
|
Bleeding |
3% |
3% |
CI 0.67-1.42 |
|
Myocardial Infarction |
2.2% |
1.0% |
CI 0.33-0.90 |
Conclusion:
The SMART-CHOICE 3 trial demonstrated the benefits of clopidogrel monotherapy when compared to aspirin therapy. It was concluded that clopidogrel monotherapy resulted in a lower risk of death, stroke or MI among patients who were at a high risk of recurrent ischemic events and who completed the standard duration of DAPT following PCI.
Alliance for Secondary Prevention After an Acute Coronary Syndrome
Speaker- Dr. Giulia Magnani
Key Highlights
Introduction:
Acute coronary syndrome is the primary cause of cardiovascular disease (CVD), which continues to be the leading cause of morbidity and mortality worldwide. Evidence from real-time studies indicates that secondary CV prevention is still not at its best, even though pharmaceutical treatment, lifestyle changes, and regulating CV risk factors diminish the recurrence of CV episodes. There is a dearth of long-term data and quantifiable advantages, despite certain studies demonstrating the short-term favourable effects of CV preventive programs, such as nurses' involvement.
Aim:
Main objective of the ALLEPRE (ALLiance for sEcondary PREvention after an acute coronary syndrome[ACS]) trial was to investigate if a well-structured, intensive, fully nurse-coordinated prevention program (NCPP) showed positive results and improvement in CV mortality, nin-fatal MI or stroke (MACE) in patients hospitalised for ACS.
Methods:
-
Design: Pragmatic, randomized, multicenter, interventional study
-
Population: 2,057 hospitalized ACS patients (STEMI, NSTEMI, UA)
-
Randomization: 1:1 prior to discharge
-
Group 1 (SOC): 1,026 patients
-
Group 2 (NCPP): 1,031 patients
-
NCPP Intervention:
-
250 full-time trained cardiology nurses
-
Centralized, in-person multidisciplinary training (medical, nursing, psychology)
-
Nurses assessed CV risk, monitored adherence, promoted lifestyle changes, and coordinated referrals
-
Primary Outcome: Composite of CV death, non-fatal MI, or non-fatal stroke over 5 years
Results:
The comparison of outcomes between both the groups is shown in the table below:
|
Events |
NCCP |
SOC |
Measures(p-value) |
|
Composite primary endpoints(MACE) |
167 |
232 |
0.0004 |
|
Cardiovascular death |
62 |
69 |
0.59 |
|
Non-fatal myocardial infarction |
96 |
156 |
0.0001 |
|
Non-fatal ischemic stroke |
20 |
26 |
0.42 |
|
Composite primary endpoint+ischemia driven coronary revascularisation |
196 |
251 |
0.005 |
|
Ischemia driven coronary revascularisation |
52 |
57 |
0.66 |
|
All cause death |
145 |
142 |
0.68 |
Conclusion:
A fully NCPP programme significantly reduced the long-term incidence of composite endpoint of CV death, non-fatal MI or stroke, in a high-risk ACS population. Though the NCPP programme has shown positive results, further studies and a cost-effectiveness analysis should be implemented before including NCPP in the healthcare system.
ACC.25, March 29 - 31, 2025, Chicago