Ph+ ALL: New Approaches for Upfront Therapy
Speaker: Marlise Luskin, Harvard Medical School
Key Highlights
Introduction to Ph+ ALL
Ph+ ALL is the most frequent genetic subtype of adult ALL, increasing with age, and primarily involves the 190-kilodalton isoform of the fusion protein. Additional cytogenetic abnormalities complicate diagnosis, sometimes resembling CML in lymphoid blast crisis. Historically, Ph+ ALL had a poor prognosis due to resistance to conventional chemotherapy, with few long-term survivors even after intensive cytotoxic regimens.
Imatinib's addition to chemotherapy initially improved survival, paving the way for TKI-based innovations.
Advancements in TKIs
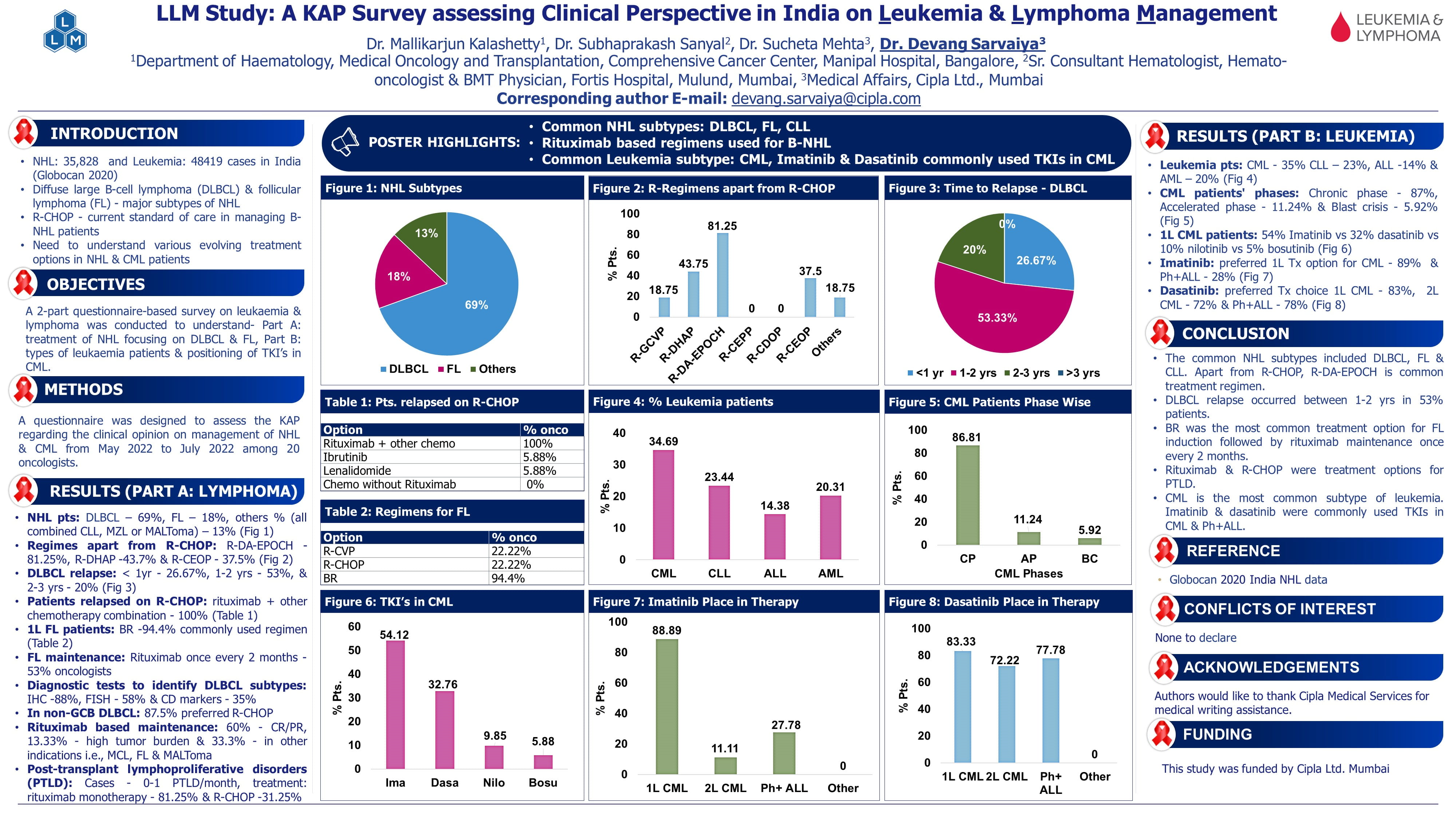
- Dasatinib vs. Imatinib: Dasatinib, a second-generation TKI, demonstrated superior event-free survival (EFS) and overall survival (OS) in children with Ph+ ALL compared to imatinib but remains vulnerable to T315I mutation resistance.
- Ponatinib's Potency: Ponatinib, a third-generation TKI, is effective against all ATP-binding site mutations, including T315I. Phase II and III trials (e.g., GIMEMA LAL 1811, PhALLCON) highlighted its efficacy in achieving molecular remission but noted significant vascular toxicities.
- Comparative Insights: Retrospective analysis suggests ponatinib provides superior outcomes compared to dasatinib in combination with hyper-CVAD, even after achieving molecular remission.
- FDA Approval: Based on the PhALLCON study, ponatinib was recently approved as first-line therapy for Ph+ ALL, marking a significant shift in treatment paradigms.
Blinatumomab Integration:
- The D'ALBA study tested a chemotherapy-free regimen using blinatumomab after a low-intensity induction with dasatinib and prednisone.
- Blinatumomab increased molecular response rates from 29% to 60% after two cycles.
- 4-year disease-free survival was 76%, and OS was 81%.
- About half the patients avoided first-remission transplantation, receiving effective therapy without it.
- Patients achieving complete molecular remission by 3 months had no relapses.
Allogeneic Transplantation:
- Allogeneic transplant showed clear benefits for patients treated before the advent of TKIs.
- Patients achieving early optimal molecular responses (MMR or MRD-negative) with imatinib, dasatinib, or hyper-CVAD regimens often did not show additional survival benefits from transplantation, though relapse risk was reduced.
- Japanese Study highlighted improved RFS and OS with transplant even in optimally responding patients treated with TKI-based regimens.
- The potential benefit of transplantation in patients receiving blinatumomab remains under investigation.
Multilineage Ph-Positive ALL
Emerging evidence indicates that the BCR-ABL transcript can arise in multipotent progenitors, leading to persistent positivity even with optimal lymphoblast clearance. Disease-free survival correlates more with immunoglobulin receptor sequencing than BCR-ABL transcript levels.
Conclusion
Dr. Luskin emphasized precision in Ph+ ALL management, advocating TKIs with reduced-intensity induction, early blinatumomab use, and stringent MRD monitoring. Transplantation is now reserved for high-risk cases, highlighting a shift toward targeted, less toxic approaches.
Ph neg. ALL: Impact of Immunotherapy in Upfront Treatment
Speaker: Matthias Stelljes, University Hospital, Muenster, Germany
Key Highlights
Introduction to Immunotherapy:
Immunotherapy has advanced outcomes in B-cell precursor ALL, with agents like blinatumomab, inotuzumab, and rituximab leading the charge. Combination of pediatric-inspired chemotherapy regimens and novel immunotherapeutic agents is transforming the treatment landscape. For instance, immunotherapy is increasingly being integrated into MRD-positive treatment protocols, with agents like blinatumomab and rituximab being incorporated for targeted approaches.
However, disparities persist, especially in elderly patients, highlighting the need for refined approaches.
CD20-Targeting Agents
Rituximab Effectiveness
|
Study |
Cycle |
Outcomes |
Notes |
|
GRAALL-2005/R |
Up to 18 |
Improved EFS, reduced relapse |
CD20-positive patients benefit |
|
UKALL14 |
4 |
No improvement |
Higher doses may be needed |
CD22-Targeting with Inotuzumab:
Efficacy Highlights:
- High remission rates (~71% MRD-negative).
- Three-year EFS: 55%; OS: 73%.
- Combination Strategies: Low-dose regimens (e.g., mini-CVD) deliver comparable outcomes with fewer toxicities.
CD19-Targeting with Blinatumomab:
- Frontline Efficacy:
- BLAST trial: 80% MRD-negative post one cycle.
- ECOG-ACRIN E1910 trial: Improved survival in MRD-positive and MRD-negative settings.
- Future Research: Address optimal cycle duration and sequencing with other immunotherapies.
Toxicity Management:
- Liver Toxicity: Caution with inotuzumab in liver-compromised patients.
- Elderly Challenges: Outcomes remain limited due to biology and reduced tolerability.
Conclusion:
Immunotherapy is revolutionizing Ph-ALL management. Inotuzumab ozogamicin is a targeted immunotherapy agent approved for the treatment of relapsed or refractory Ph- ALL. Agents like blinatumomab and inotuzumab allow tailored, less chemotherapy-dependent strategies. Comparative trials are essential to refine regimens for maximum efficacy and safety.
Transplant in ALL: Who, When, and How?
Speaker: Partow Kebriaei, MD Anderson Cancer Centre
Key Highlights
Dr. Partow Kebriaei explored the role of hematopoietic stem cell transplantation (HSCT) in ALL, focusing on three central aspects: patient selection, timing of transplant, and conditioning regimens. The session emphasized how advancements in targeted therapies and immunotherapies are reshaping the transplant landscape.
Patient Selection for Transplant:
High-Risk Features: HSCT in first remission is recommended for patients with high-risk features:
- Genetics: KMT2A rearrangements, hypodiploidy, TP53 mutations.
- Molecular Risk: Persistent MRD in Ph-like ALL.
- T-ALL Subtype: Early T-cell precursor (ETP) ALL, with poor standard therapy outcomes.
Role of MRD:
Early MRD clearance, assessed via NGS or flow cytometry, indicates a lower likelihood of requiring HSCT in first remission unless other high-risk features exist. Persistent MRD is a critical determinant for transplant consideration.
Timing of Transplant:
First vs. Second Remission:
- High-risk groups benefit from HSCT in first remission.
- Immunotherapies (e.g., blinatumomab, inotuzumab, CAR-T cells) enable some patients to defer HSCT to second remission if MRD negativity is achieved.
CAR-T Cell Consolidation: For relapsed/refractory patients, CAR-T cell therapy followed by HSCT deepens remission, particularly in MRD-positive settings.
Conditioning Regimens and Innovations:
- Myeloablative Conditioning:
- TBI-based regimens remain standard for younger patients.
- Non-TBI regimens reduce toxicity and are considered for older adults.
- Novel Approaches:
- Incorporating inotuzumab into conditioning regimens improves outcomes but increases toxicity risks.
- Research is ongoing into de-escalated conditioning regimens for MRD-negative patients to reduce treatment-related toxicity.
Key Data Highlights:
- ALLIANCE A041501 Study: High MRD clearance rates with inotuzumab, but increased toxicity warrants caution.
- ECOG-ACRIN E1910 Trial: Blinatumomab combined with chemotherapy significantly improved outcomes, supporting its role in achieving MRD negativity pre-HSCT.
- Ph-Positive ALL: HSCT may be omitted for MRD-negative patients responding well to TKIs. However, those with high-risk features, such as IKZF1 mutations, benefit from transplant.
Challenges and Open Questions:
- MRD Monitoring:
- Determining the optimal timing and method (NGS vs. flow cytometry) for MRD assessment.
- Peripheral blood-based MRD monitoring offers potential for simplified longitudinal evaluations.
- Genetic Profiling: Refining transplant decisions by integrating genetic risk stratification with MRD data.
- CAR-T Cell Integration: Defining criteria for HSCT post-CAR-T therapy and evaluating long-term outcomes.
- Conditioning Regimen Refinement: Balancing efficacy and toxicity in novel or intensified regimens, especially for high-risk or refractory patients.
Conclusion
HSCT remains integral to ALL treatment for patients with adverse genetic features or persistent MRD. However, advances in immunotherapy and precision medicine are redefining its role, with the potential to delay or omit transplant in select cases. Ongoing prospective studies are essential to optimize MRD-based strategies, conditioning regimens, and post-transplant care in this evolving treatment paradigm.
ASH Annual Meeting and Exposition, 7-10 December 2024, San Diego, California