Speaker- Laurie HENRY
Endometriosis, a condition associated with infertility, is influenced by multiple factors, including dyspareunia, mechanical characteristics, ovarian reserve, impaired ovulation, and endometrial receptivity. A comprehensive understanding of these complexities is essential for effectively managing fertility in patients with endometriosis. The decline in ovarian reserve observed in women with endometriosis and endometriomas may result from both the presence of the cyst and surgical interventions. However, the specific contributions of each still need to be clarified.
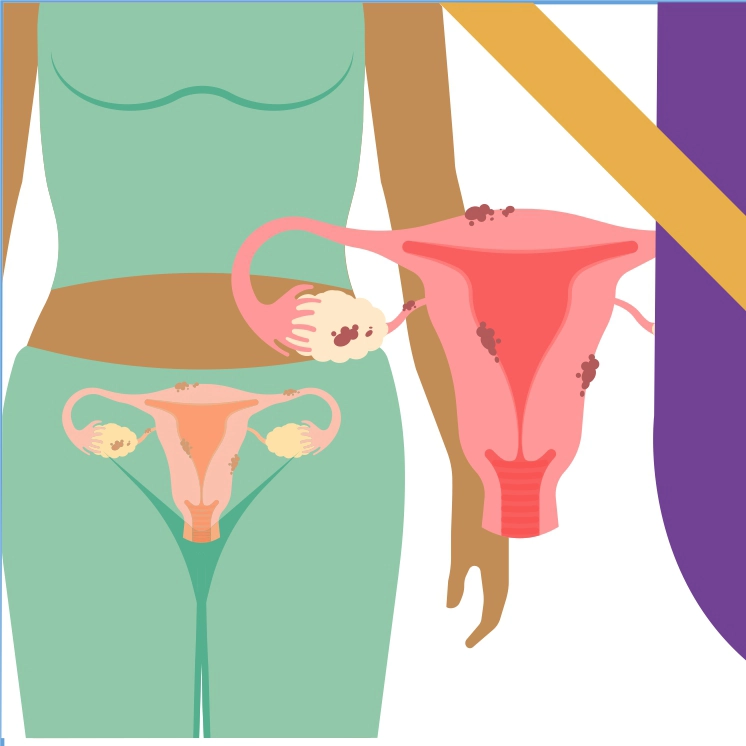
Endometriotic cysts have lower follicular density than normal ovaries due to fibrotic transformations in the cyst wall and surrounding ovarian tissue. These cysts contain elevated levels of free iron, reactive oxygen species, proteolytic enzymes, and inflammatory mediators, which influence adjacent endometriotic cells, leading to gene expression changes and genetic mutations. The minimal physical barrier separating cyst contents from normal ovarian tissue allows for the diffusion of cystic and proteolytic substances, leading to smooth muscle metaplasia, follicular depletion, and intra-ovarian vascular damage.
Research indicates that the ovarian endometrioma microenvironment can activate dormant primordial follicles, reducing their numbers. Surgical removal may exacerbate this hyperactivation, further diminishing ovarian reserve. Several signaling pathways contribute to this increase. Patients with endometriomas have lower levels of Anti-Müllerian Hormone (AMH), with significant differences observed between endometriomas and benign ovarian cysts.
Endometriosis can impact oocyte quality, contributing to structural abnormalities and reduced mitochondrial content. Research, such as the meta-analysis by Sonia Gayat Lafuente, indicates that these effects generally do not significantly affect fertilization and blastulation rates. However, in patients with endometriomas, there is often a lower yield of total retrieved oocytes and metaphase II oocytes, producing fewer high-quality embryos.
Endometriosis is a growing concern among women aged 30 to 35, with the peak incidence occurring around age 30 due to a decline in ovarian reserve. Anti-Müllerian Hormone (AMH) levels are a reliable indicator of ovarian reserve, and higher levels during oocyte cryopreservation and earlier efforts lead to better outcomes and successful conception. Preservation procedures should be performed before ovarian surgery to maximize reproductive potential. Endometriomas larger than 4 cm do not significantly impact outcomes related to AMH concentrations or metaphase II oocytes, provided surgical intervention is not required.
Surgery for endometriomas can impact ovarian reserve differently depending on factors such as the surgeon's expertise, the type of surgery performed, and the techniques utilized. Surgical inflammation may adversely affect ovarian function, and repeated procedures can compound these risks over time. As fertility declines with age, with the peak fertility rate shifting from ages 25-29 to 30-34 as of 2022, fertility preservation becomes particularly critical for patients with endometriosis. It is recommended to consider preserving ovarian reserve ideally before the age of 36 and before any surgical intervention for endometriomas when ovarian function is optimal.
Somi Gleana's 2015 study suggests fertility preservation for patients with endometriosis, especially those with bilateral endometriomas, previous surgery, or small lateral excisions. Nicole Zanger's study found significant variability in fertility preservation practices across Europe. The European Society of Human Reproduction and Embryology (ESHRE) guidelines in 2020 suggest severe endometriosis increases the risk of premature ovarian insufficiency and lowers AMH levels, which surgical interventions can impact. The ESHRE 2022 guidelines recommend discussing fertility preservation options for women with extensive endometriosis.
Preserving fertility before surgery, especially for endometriosis, offers benefits like procedural safety and improved reproductive prognosis. However, weaknesses are areas for improvement cited data, lack of international recommendations, inconsistent coverage by public health insurance, and comprehensive cost-benefit studies. Increased awareness and collaboration among specialists can enhance outcomes for women with endometriosis. Managing endometriosis patients in specialized centers is crucial to mitigate surgical risks to ovarian reserve.
Endometriosis patients should be treated in specialized centers to mitigate surgical risks and consider queer preservation when clinically appropriate. Determining when to offer preservation and whether it is part of a short-term or long-term strategy is crucial. Before considering surgery for patients without a short-term desire for pregnancy, it is essential to discuss the feasibility of fertility preservation strategies. It is also important to use vitrified oocytes or embryos after surgery or to store them for future attempts. It is crucial to provide patients with the necessary information to consent.
Endometriosis is a common chronic condition that significantly impacts fertility, especially among women of reproductive age, often leading to diminished ovarian reserve. Surgical treatments can further exacerbate this decline. To mitigate risks, patients should be managed by multidisciplinary teams and specialized surgeons who are experienced in treating endometriosis. While fertility preservation techniques are effective, they should be carefully considered for patients with endometriosis due to the current lack of international consensus and comprehensive cost-benefit studies. Specifically, patients with bilateral endometriomas or recurrent disease on the contralateral ovary should be informed about and offered fertility preservation options as part of their treatment planning.
European Society of Human Reproduction and Embryology, July 7-10, Amsterdam, The Netherland

.svg?iar=0&updated=20230109065058&hash=B8F025B8AA9A24E727DBB30EAED272C8)

.webp?updated=20240806062824)