ESHRE 2024: An Individualized Approach to the Treatment of Recurrent IVF Failure
Speaker Rekha Pillai
The discussion focused on defining recurrent in-vitro fertilization (IVF) failure and personalizing treatment for better patient counseling and tailored interventions. The Canadian Fertility and Andrology Society noted the lack of a universal definition. A UK publication defined recurrent implantation failure as no implantation after two consecutive Intracytoplasmic sperm injection (IVF/ICSI) cycles or after transferring four pre-wastage embryos or two good-quality blastocysts. An (ESHRE) European Society of Human Reproduction and Embryology survey found the most common guideline to be after three consecutive embryo transfers (fresh and frozen). However, professional organizations varied: The American Society for Reproductive Medicine (ASRM) had no criteria, the Canadian society acknowledged the lack of a universal definition, and the British Fertility Society defined it in 2022 as three consecutive good-quality embryo transfers. These definitions ignored factors like oocyte and uterine age, systemic conditions, and endometrial issues. ESHRE's 2023 recommendations faced challenges due to varying definitions and limited data. Their guidelines provide a foundation but emphasize the need for further discussion.
The approach to individualizing recurrent IVF failure used prediction models and thresholds. Key models included the Dylan model and the IVF Predict tool. ESHRE provided a complex formula and a simplified chart considering embryo ploidy, woman's age, and transfer numbers. ESHRE recommended investigations: reassessing lifestyle factors, endometrial thickness, antiphospholipid screening, hysteroscopy, 3D ultrasound, and tests for chronic endometritis, thyroid function, and progesterone levels. They did not recommend vitamin D testing, microbiome profiling, or various immune cell assessments. Recommended interventions: optimizing lifestyle factors, genetic counseling, pre-implantation genetic testing for chromosomal anomalies, and managing thin endometrium. Antibiotics for chronic endometritis, pre-implantation genetic testing for aneuploidy, and blastocyst-stage embryo transfer were suggested. Treatments like vitamin D, endometrial scraping, and immune-related therapies were not recommended. ESHRE emphasized personalized care, kindness, support, and honest patient communication during this challenging time.
The relevance of lifestyle factors in Assisted Reproductive Technology (ART) is highlighted, with low-quality evidence suggesting that factors like cigarette smoking, alcohol, and caffeine intake may impact success rates. These findings are extrapolated from ART patients, which includes logical implications for those experiencing Recurrent Implantation Failure (RIF). Body Mass Index (BMI) was highlighted as a relative risk factor for IVF failure. However, investigating and treating vitamin D deficiency isn't recommended by ESHRE, despite a 2018 UK meta-analysis suggesting potential benefits in ART patients. Regarding endometrial thickness, a systematic review of 22 studies indicated higher success rates with thickness above seven millimeters. A retrospective study with a large patient cohort suggested clinical pregnancy rates were higher above 8mm, though it didn't significantly affect live birth rates in multivariate analysis.
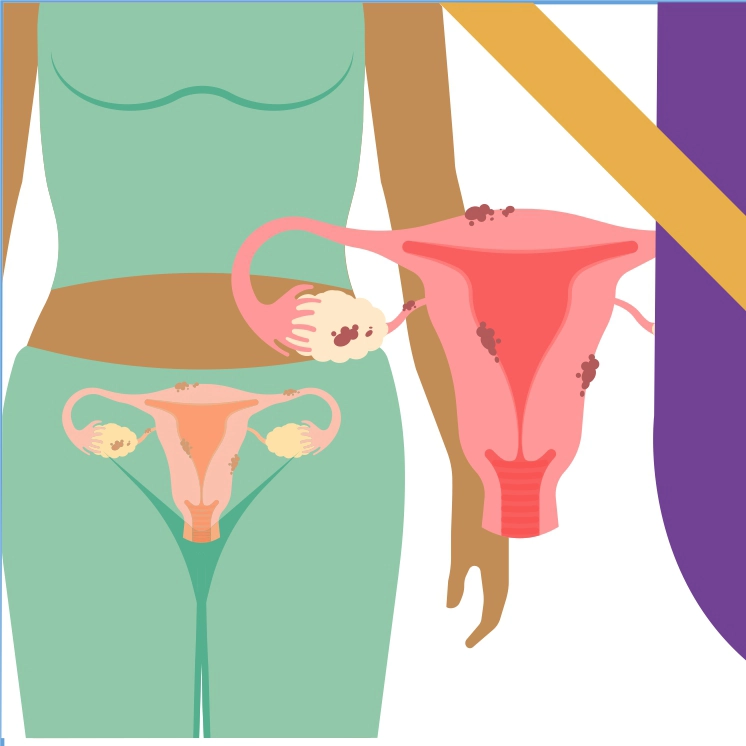
Atta et al.'s recent retrospective study found no link between endometrial thickness and live birth rates, supported by the Receiver Operating Characteristic (ROC) curve and log regression analyses. ESHRE advises reassessing thickness due to absorption variability, suggesting estrogen supplementation if thin. Platelet-rich plasma and intrauterine Genetic Silencing and Substitution (GSS) therapies show potential but need more study; hysteroscopy is recommended for suspected Asherman syndrome. Thrombophilia increases clotting risk and impairs implantation; inherited types show no RIF association, but recent studies link Antiphospholipid Syndrome (APS) screening to RIF. Genetic factors like chromosomal abnormalities are more prevalent in RIF cases, warranting karyotyping, genetic counseling, and possibly pre-implantation genetic testing for management.
Pre-implantation genetic testing for aneuploidy (PGTA) helps deselect embryos with whole chromosome abnormalities. A Cochrane review in 2020 found no significant improvement in live birth rates or miscarriage reduction, primarily using Fluorescence In Situ Hybridization (FISH) technology. New technologies like Comparative Genomic Screening (CGS) and Next-generation sequencing (NGS) promise to reduce miscarriages and embryo transfer numbers, though live birth rates remain unaffected. In the UK, the Human Fertilisation and Embryology Authority (HFEA) regulates fertility clinics and uses a color-coded system to inform patients about treatment benefits. HFEA's recent recommendation on PGTA indicates it may reduce miscarriage risk (green) for most fertility patients, but its benefit for older women remains uncertain (grey). ASRM in the US advises caution, citing limited benefits in lower-risk populations.
In 2022, a systematic review from Italy indicated chronic endometritis could reduce live birth rates, suggesting treatment might help. Concurrently, a review from China found it increased clinical pregnancy rates but not live births, possibly due to inconsistent test standards. New DNA tests aim to improve diagnostic accuracy. Endometrial receptivity testing uses gene panels from biopsies to assess implantation windows, focusing on single factors rather than the complex nature of receptivity. Recent multicentre studies suggested personalized embryo transfer using Endometrial receptivity tests may reduce live births compared to unguided transfers, with some benefits in per-protocol analyses. ESHRE advises caution due to limited data, recommending exploration of specific aspects of endometrial function testing. Hysteroscopy and 3D ultrasound are used to assess uterine cavities, with hysteroscopy aiding in identifying and correcting anomalies like polyps or fibroids, potentially improving live births after recurrent implantation failure. The impact of adenomyosis on implantation remains unclear, with mixed findings on treatments like Gonadotropin-Releasing Hormone (GnRH) agonists. The British Fertility Society advises the removal of polyps and submucosal fibroids, but intramural myomas are discretionary based on individual cases. Hydro salpingectomy is preferred over tubal occlusion or aspiration for improving fertility outcomes. Thyroid function tests target a Thyroid Stimulating Hormone (TSH) level of 4.4 in assisted reproduction, considering thyroid antibodies. Premature progesterone rises may disrupt endometrial synchrony, with variable cutoff levels affecting implantation.
Validation of cutoff levels for hormonal assays typically involves local clinic validation to determine thresholds suitable for their specific equipment and patient population. Recent studies suggest a cutoff of 9.2 for certain hormonal levels, but improvements in outcomes like live birth rates remain inconclusive. Recommendations advise clinics to adjust cutoffs based on their validation processes and current study insights.
European Society of Human Reproduction and Embryology, July 7-10, Amsterdam, The Netherlands