SIU 2024: (MC-12) Intermediate Risk Disease – Who Needs Induction and Maintenance and Active Surveillance
Speaker: Dr. Deepak Krishnappa, India
Important Takeaways
-
Dr. Krishnappa emphasised the complexity of intermediate risk NMIBC, describing it as a "gray area" between low and high risk.
-
Risk Factor-Based Treatment Strategy: The treatment for intermediate risk patients depends on the number of risk factors present.
-
Treatment Outcomes and Recurrence Rates: Recurrence rates vary significantly based on risk factor count, with higher factors leading to higher recurrence.
-
Chemotherapy vs. BCG: While BCG may help prevent both recurrence and progression, chemotherapy focuses more on recurrence.
-
Institutional Practices: Dr. Krishnappa shared insights into how his centre in Bangalore uses Gemcitabine-Doxorubicin combination therapy for NMIBC cases.
Key Highlights
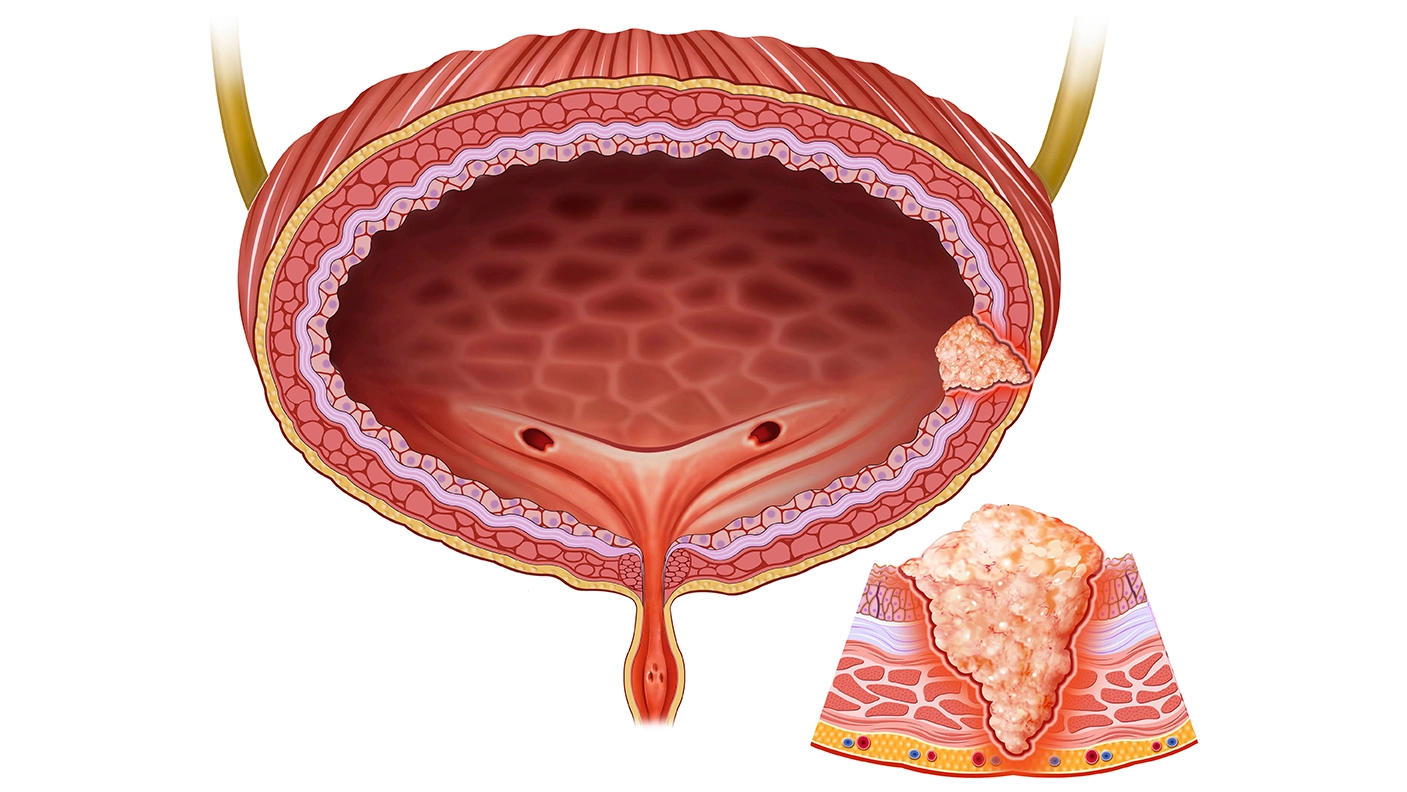
Intermediate-Risk Classification and Subgroups:
Intermediate-risk NMIBC includes cases that don’t fully meet high or low-risk criteria. For example, high-grade TA tumours, often classified as intermediate by EAU and AUA guidelines, might warrant a closer look given their potential aggressiveness.
The International Bladder Cancer Group (IBCG) further categorises intermediate-risk patients based on the number of risk factors (0, 1-2, or >3), allowing clinicians to tailor management strategies more precisely.
Treatment Recommendations Based on Risk Factor Count:
-
Zero Risk Factors: A transurethral resection of the bladder tumour (TURBT) followed by a single postoperative dose of chemotherapy is usually sufficient.
-
One or Two Risk Factors: For patients with one or two risk factors (such as tumour size >3 cm or recurrence within a year), a 6-week course of induction chemotherapy is recommended, with follow-up BCG therapy if recurrence occurs.
-
More than Three Risk Factors: Patients with three or more risk factors should receive BCG therapy as induction and a one-year maintenance schedule. Should recurrence happen after this, options include gemcitabine-docetaxel combination or hyperthermic intravesical chemotherapy (HIVEC).
Recurrence and Progression Rates:
Recurrence rates for intermediate-risk patients increase proportionally with the number of risk factors. For example, recurrence rates at five years range from 38% for zero risk factors to 78% for those with three or more.
Induction vs. Maintenance:
A randomised study comparing one-year to three-year BCG maintenance in intermediate-risk patients showed no significant difference in outcomes, suggesting that one-year maintenance may be adequate.
Chemotherapy versus BCG: While studies have found similar recurrence prevention rates between chemotherapy and BCG in intermediate-risk patients, BCG remains the preferred choice for those with high recurrence risks.
T1 Low-Grade Disease Classification Debate:
Dr. Krishnappa noted that T1 low-grade cases are rare and often represent cases misclassified at pathology. When they do occur, they may not fit well into the typical intermediate-risk category, sparking debate on whether they belong in a high-risk grouping instead.
Three-Month Recurrence as a Predictor:
Patients showing recurrence within three months’ post-treatment are at higher risk for further recurrence. Those who remain disease-free at three months have a significantly reduced recurrence risk, emphasising the importance of early surveillance.
This talk underscored the need to personalise treatment plans in intermediate-risk NMIBC and adapt therapy based on recurrence risk, available resources, and individual patient profiles. The discussion confirmed that recurrence prevention remains the main treatment objective in intermediate-risk patients, while progression prevention is prioritised in high-risk cases.
Société Internationale d'Urologie Congress, 23-26 October 2024, New Delhi, India.