RED VELVT Study: Warfarin vs. DOAC for the Treatment of Left Ventricular Thrombi
7 Jul, 20
Background
Patients with ischemic and nonischemic cardiomyopathies have a high risk of left ventricular (LV) thrombi. Although anticoagulation may cut down the risk of stroke or systemic embolism (SSE), there is lack of data on the effectiveness of direct oral anticoagulants (DOACs) for this indication. The embolic outcomes of DOACs vs. warfarin for LV thrombi have also not been studied until now.
Aim
The Retrospective Evaluation of DOACs and Vascular Endpoints of the Left Ventricular Thrombi (RED VELVT) study compared the embolic outcomes associated with DOAC use vs. warfarin use for the treatment of LV thrombi.
Patient Profile
- Patients with echocardiographically diagnosed LV thrombi (n=514)
Methods
Study Design
- A multicenter (conducted across 3 tertiary centers), retrospective study
Exposures
- Type and duration of anticoagulant use
Outcome
- Clinically apparent SSE
Follow-up
- Median period: 351 days
Results
- Mean age of the study population was 58.4 years, 379 patients were males.
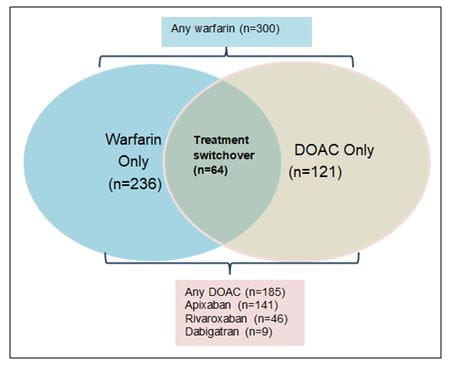
- Of the entire study population, 300 were treated with warfarin and 185 were treated with a DOAC. Sixty-four patients switched treatment between these groups such that 236 patients were treated exclusively with warfarin (warfarin-only group) and 121 were treated exclusively DOACs (DOAC-only group)
Figure 1: Anticoagulation strategy used during the study
- The most common cause for switch over from warfarin to DOACs was convenience (19.2%) and the most common cause of switch over from DOACs to warfarin was cost (31.6%)
- Amongst the 185 patients treated with DOACs, 76.2% (n=141) received apixaban, 24.9% (46) received rivaroxaban and 4.9% (n=9) received dabigatran.
- During the median follow-up of 351 days, 54 SSE events (36 ischemic strokes and 18 systemic emboli) occurred. Of these, 17 occurred among patients taking a DOAC and 14 occurred among patients taking warfarin.
- As per an unadjusted analysis, DOAC treatment vs. warfarin use was associated with SSE (hazard ratio [HR], 2.71; 95%CI, 1.31-5.57; P = 0.01). Prior SSE was also associated with SSE (HR, 2.13; 95%CI, 1.22-3.72; P = 0.01).
- Anticoagulation with DOAC vs. warfarin (HR, 2.64; 95%CI, 1.28-5.43; P = 0.01) and prior SSE (HR, 2.07; 95%CI, 1.17-3.66; P = 0.01) remained significantly associated with SSE even in a multivariable analysis.
- Considering that LV dysfunction is associated with a high death risk, the competing risk was calculated by evaluating the risk of death as per the anticoagulant strategy. As per the unadjusted analysis, treatment with DOACs vs. warfarin was significantly associated with death or SSE (HR; 1.55, 95% CI; 1.05-2.30; p=0.03).
Conclusions
- Amongst patients with LV thrombi, DOAC treatment was associated with a higher risk of SSE as compared with warfarin use, even after adjusting for various covariates.
- Nearly 43.9% patients treated with anticoagulants received off-label DOACs at least for some period during their treatment course.
- The findings from this study put under scrutiny the assumption of DOAC equivalence with warfarin for treating LV thrombi. Further prospective randomized clinical trials are warranted to determine the most effective treatment strategies for LV thrombi.
JAMA Cardiol. Apr 22, 2020 (Published Online); doi:10.1001/jamacardio.2020.0652.