Background
There is discrepancy on the definition of optimal timing of invasive coronary angiography (ICA) and revascularization in patients with non-ST-segment elevation (NSTE) acute coronary syndrome (ACS). Moreover, the extent to which an early ICA (conducted within 14 hours of NSTE-ACS diagnosis) would be beneficial for the patient has not been determined completely.
Aim
VERDICT (Very Early Versus Deferred Invasive Evaluation Using Computerized Tomography) trial determined whether a strategy of very early ICA and possible revascularization within 12 hours of diagnosis would be associated with superior clinical outcomes as against an invasive strategy performed within 48 to 72 hours
Patient Profile
- Adult patients (age above 18 years) with a clinical suspicion of ACS in whom ICA was indicated and ≥1 of the following high-risk criteria was present:
- ECG changes indicating new ischemia (new ST segment depression, horizontal or down sloping ≥0.05 mV in 2 consecutive leads, or T-wave inversion >0.01 mV in 2 leads with prominent R wave or R/S ratio >1)
- An increase in coronary markers of ischemia (troponin)
Methods
Study Design
- Prospective, multicenter, open label, parallel group, randomized controlled trial
Randomization
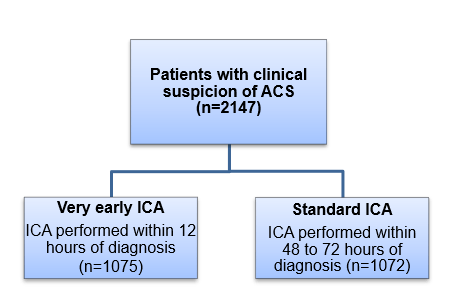
- Patients were randomized 1:1 as follows:
- Patients were assessed for clinical outcomes after ≥18 months
Procedures
Medical Treatment
- At time of hospitalization and before randomization, all patients received oral ?-blockers, statins, a loading dose of P2Y12 inhibitor (clopidogrel 600 mg or ticagrelor 180 mg), aspirin 300 mg, and subcutaneously administered fondaparinux 2.5 mg daily unless contraindicated.
Coronary Angiography and Revascularization
- ICA was performed as per the guidelines and clinical practice at the individual invasive center
- Patients undergoing PCI received unfractionated heparin to obtain an activated clotting time between 250 and 300 seconds.
- Further addition of bivalirudin or glycoprotein IIB/IIIA inhibitors to the treatment regimen was at the discretion of the operator
Endpoints
Primary Endpoint
- A combination of all-cause death, nonfatal recurrent myocardial infarction (MI), hospital admission for refractory myocardial ischemia, or hospital admission for heart failure (HF)
Secondary Endpoint
- Invasive procedure complications during index hospitalization (procedure related death, bleeding as per the “Bleeding Academic Research Consortium” [BARC] criteria, procedure-related nonfatal acute MI [AMI], stroke, or transient ischemic attack) in addition to the occurrence of each of the following events at any time after randomization: death, nonfatal AMI, admission for refractory myocardial ischemia, repeat coronary revascularization, or hospital admission for HF
Follow-up after Randomization
- Median follow-up of 4.3 years
Results
- ICA was performed at a median of 4.7 hours after randomization in the very early invasive strategy group, and after 61.6 hours in the standard care invasive strategy group.
- Among patients with significant coronary artery disease identified by ICA, 88.4% patients from the very early ICA group underwent coronary revascularization as compared to 83.1% patients from the standard invasive care group.
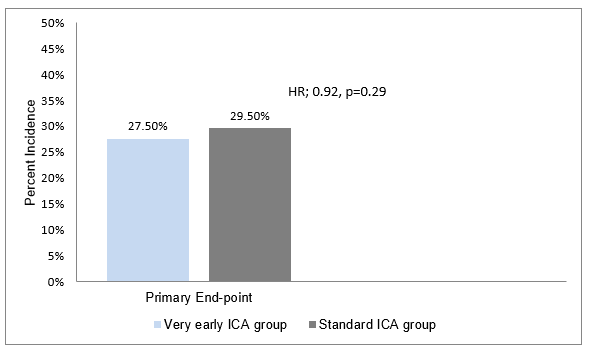
- The incidence of primary endpoint was similar in both the study groups (27.5% [very early ICA group] vs. 29.5% [standard care group], hazard ratio [HR]; 0.92; 95% CI; 0.78–1.08) (Figure 1).
- A very early invasive treatment strategy reduced the incidence of primary outcomes in patients with a GRACE risk score (Global Registry of Acute Coronary Events) >140 by 19% vs. those with the standard invasive treatment (HR; 0.81; 95% CI; 0.67–1.01, P value for interaction = 0.023).
- With regards to secondary endpoint, a very early ICA strategy was associated with a 27% risk reduction in the incidence of non-fatal AMI (8.4% vs. 11.2%, HR: 0.73, p=0.025), and 22% risk reduction in the incidence of HF (9.2% vs. 11. 8%, HR; 0.78, p0.06) as compared to the standard invasive treatment.
Conclusions
- A very early invasive coronary evaluation strategy (within 4.7 hours of diagnosis) does not improve overall long-term clinical outcome as compared to the standard invasive strategy (conducted within 2 to 3 days) in NSTE-ACS patients.
- Nevertheless, very early invasive therapy improved long-term outcomes in patients at highest risk.
Circulation. 2018; 138: 2741–750.