Nebulization is the process by which a liquid medication is converted into a fine mist that can be inhaled. The device that is used to convert the liquid drug into aerosol droplets suitable for patients to inhale is known as a 'Nebulizer'.
A Practical Guide to Nebulization Therapy
A Practical Guide to Nebulization Therapy
Introduction to Nebulization
What is Nebulization?
What is the Method of Inhalation with a Nebulizer?
The patient should be instructed to sit upright, take steady breaths (tidal breathing), and to not talk during the nebulization. Steady normal breathing interspersed with occasional deep breaths is likely to be optimal. It should be noted that the nasal passages effectively filter droplets delivered from the nebulizer. Hence, oral breathing is preferred over nasal breathing.
What are the Advantages of Nebulizer Therapy?
- It does not require coordination between inspiration and actuation as it uses normal tidal breathing
- It is the most convenient way of delivering high doses of inhaled medication.
- In acute severe asthma, oxygen can be used to nebulize the drug.
- Only 2% of the aerosol from the nebulizer is deposited in the mouth, compared to 60-80% oral deposition from metered dose inhaler (MDI) (when not using a spacer device).
- It can be used by any age group
What are the Clinical Indications for the Use of Nebulizer Therapy?
- In acute attacks of asthma or COPD exacerbations, nebulized treatment is usually employed
- Patients not able to or too sick or incapable of managing handheld inhalers
- Drugs not available in handheld inhaler (eg: arformoterol, N-acetylcysteine)
- Need for a large drug dose
- Patient preference: Many patients may prefer nebulizer therapy over other inhaler devices.
- Practical convenience
Types of Nebulizers
How Does the Nebulizer Work?
Nebulizers used in aerosol drug delivery produce a polydisperse aerosol where most of the drug is released in the form of particles, which are 1 to 5 microns in diameter. The nebulizer works by using the compressor to pump the atmospheric air at high pressure through the liquid medicine, thus converting it into a mist, which can then be easily inhaled.
What are the Different Types of Nebulizers Available?
Nebulizers exist in many different forms. Based on the method of aerosol generation, they may be broadly divided into jet and ultrasonic nebulizers. Of these, the jet nebulizers are widely used. Newer nebulizer designs available are mesh nebulizers, breath-enhanced nebulizers, and breath-actuated nebulizers; some also have aerosol storage bags to minimize aerosol loss during exhalation.
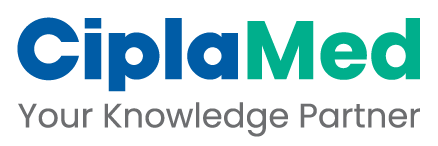
How Does a Jet Nebulizer Work?
In a jet nebulizer, the compressor pumps atmospheric air at high pressure through a very narrow hole, known as a venturi. In the venturi, the pressure falls and the air velocity increases greatly, thereby creating a cone-shaped air flow. This air flow projects at high velocity out of the ends of a narrow liquid feed tube or concentric feeding system, creating a negative pressure at this point. As a result of this fall in pressure, the liquid in the nebulization chamber is sucked up (a process known as the Bernoulli Effect) and is drawn out into fine ligaments. The ligaments then collapse into droplets under the influence of the surface tension. This primary generation is known as atomisation.
Atomisation typically produces droplets of 15-500 microns in diameter. A nebulizer may be distinguished from a simple atomizer by the incorporation of baffles, which selectively remove large droplets from an outgoing spray. Coarse droplets impact on the baffles while smaller droplets are inhaled or may land on the internal walls, returning to the chamber for re-nebulization. Baffle design, therefore, has a critical effect on the droplet size.
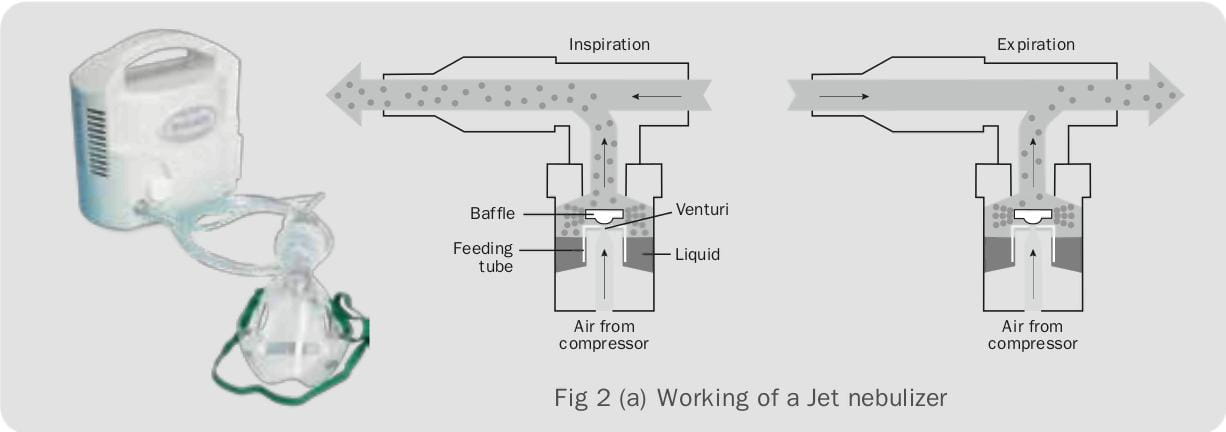
How Does an Ultrasonic Nebulizer Work?
The ultrasonic nebulizer uses a rapidly vibrating piezoelectric crystal to produce aerosol particles. Ultrasonic vibrations from the crystal are transmitted to the surface of the drug solution, thereby creating upright wave patterns in the solution. Droplets break free from the crests of these waves and are released as aerosol. The size of the droplets produced is inversely proportional to two-thirds of the power of the acoustic frequency. As in jet nebulizers, baffles within the ultrasonic nebulizer break the large droplets and much of the aerosol produced also impacts on the baffles, falling back into the drug reservoir.
What are the Differences Between Ultrasonic and Jet Nebulizers?
Ultrasonic nebulizers are generally smaller, quieter and take lesser time to use.
Jet nebulizers are by far the most common type of nebulizers used worldwide. Advances in design have improved their efficiency such that the higher mass output and shorter nebulization times seen with ultrasonic nebulizers may no longer be important discriminating factors.
What are the New Nebulizer Designs Available that Enhance Nebulizer Performance?
In recent years, several new nebulizer designs have become available, which decrease the amount of aerosol lost during the expiratory phase. These include reservoir bags to collect the aerosol during the expiratory phase, the use of a vented design to increase the nebulizer output during the inspiratory phase (breath-enhanced nebulizers), and nebulizers that only generate aerosol during the inspiratory phase (breath-actuated nebulizers). Because these designs improve drug delivery to the patient, they have the potential to reduce treatment time, which should thereby improve patient compliance with nebulizer therapy. Although, several new designs show improved nebulization performance, their cost-effectiveness remains to be determined.
What is a Mesh Nebulizer?
Several manufacturers have developed aerosol devices that use a mesh or plate that has multiple apertures to produce an aerosol. These devices use a vibrating mesh or a vibrating horn.
Nebulization with a mesh nebulizer is dependent on the characteristics of the liquid drug used; these nebulizers may be unsuitable for viscous liquids, which suggest that matching the formulation to the device may be important for these aerosol generators.
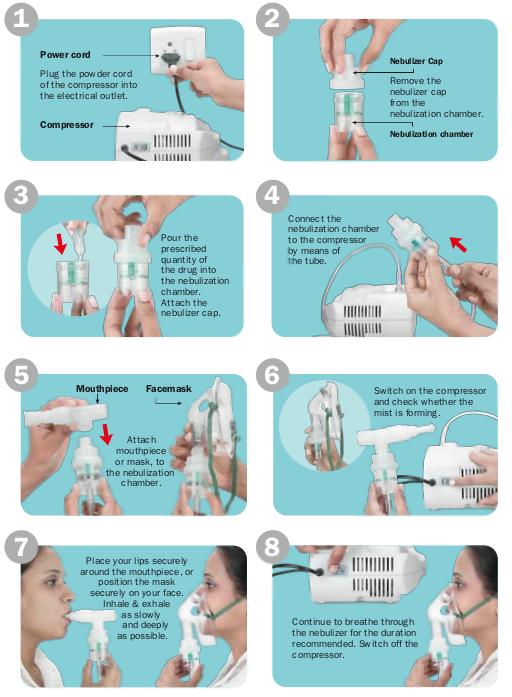
Assembly & Drug Administration Through Nebulizers
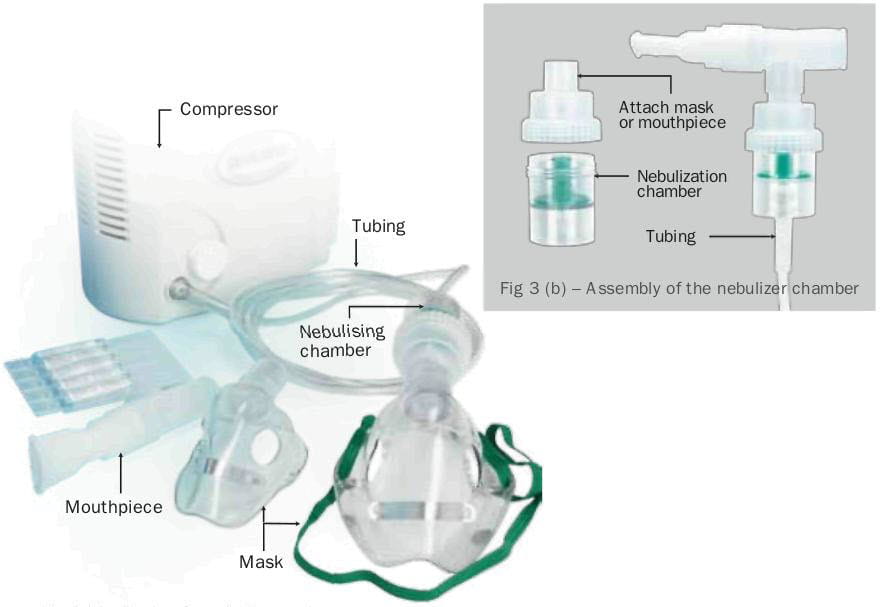
What are the Parts of a Nebulizer System?
A nebulizer system consists of different parts such as a compressor, tubing, nebulization chamber, and a mouthpiece (or) a face mask.
The compressor is a portable pump that powers the nebulizer. The nebulization chamber is a small, specially designed container into which the liquid drug to bem nebulized is put and through which air is blown to make a mist. The tubing connects the compressor to the nebulizing chamber. The mist produced can be inhaled via either a mouthpiece or a face mask. Sometimes, the mouthpiece is made available in a T shape and is called a T-piece.
Where is the Drug Placed in the Nebulizer System?
The liquid drug to be nebulized is put in the nebulization chamber, which is then attached to the compressor with the help of a connecting tube. A mask or a mouthpiece is then attached to the chamber to aid inhalation.
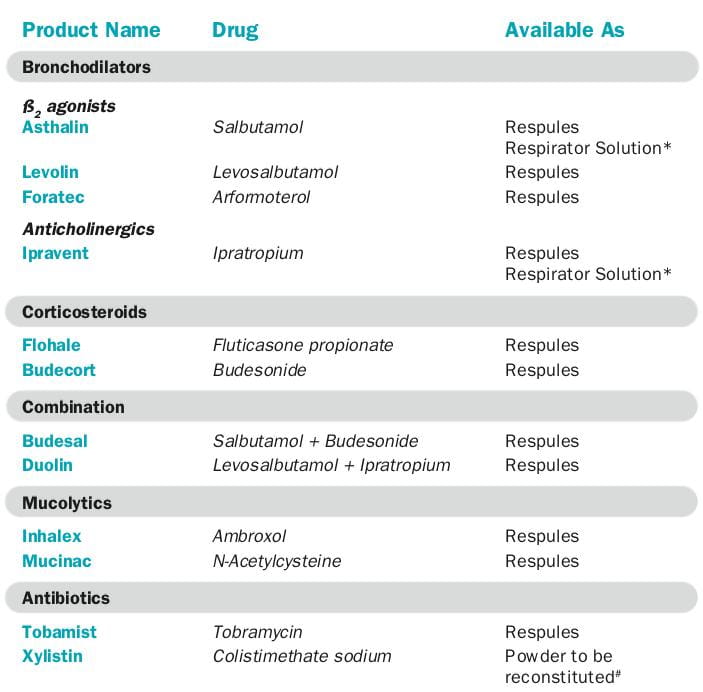
What are the Different Types of Liquid Drugs Used in Nebulization?
Most liquid drugs for nebulization fall into two physiochemical categories, i.e., solutions and suspensions.
Solutions
Solutions contain a drug that is dissolved in saline or, occasionally, in other liquids. In solutions, the entire drug is homogeneously dispersed throughout all the droplets
Suspensions
Suspensions contain a drug that is not soluble in water or other respirable liquids; they exist as a mixture of small drug particles suspended in liquid. Currently 4 groups of drugs are available for nebulization. These include bronchodilators, steroids, antibiotics and mucolytics.
What is the Optimal Volume of the Drug to be Put in the Nebulization Chamber?
The optimal volume of the drug (also known as fill volume) to be put in the nebulization chamber is approximately 2 ml-4 ml. Nebulizing chambers have different maximum fill volumes; the volume of drug solution must not exceed the maximum fill volume.
What is a 'Respule'?
A 'respule' is an ampoule containing the liquid drug to be nebulized. The drug is already pre-diluted and, hence, can be used directly. The respule should be broken and the liquid drug should be poured into the nebulization chamber for nebulization.
What is a 'Respirator Solution'? How Should it be Diluted?
A 'respirator solution' contains the drug to be nebulized in concentrated form. Before use, it is important to dilute this drug with normal saline, depending on the amount of drug required.
This concentrate should be diluted in a ratio of 1 part of drug solution: 3 parts of normal saline (0.9% sodium chloride solution). Care should be taken that after diluting, the fill volume should not exceed the recommended volume of 2-4 ml.
Can Distilled Water or Tap Water be Used to Dilute the Respirator Solution?
No, it is not recommended to use any other solution apart from normal saline, as distilled water or tap water contains certain elements that could irritate the airways.
What is the Optimal Driving Gas Flow Rate for Nebulization?
Most jet nebulizers are now designed to work at a gas flow rate of 6-10 litres per minute.
Can the Drug be Nebulized with Oxygen Instead of Air?
The drug can also be nebulized with oxygen (from an oxygen cylinder) at a standard flow rate of 6-8 litres per minute or a higher flow rate exceeding 8 litres per minute.
What is the Optimal Time for Nebulization? When Should it be Stopped?
The optimal nebulization time, i.e., from nebulization start to nebulization end, should not exceed 10 minutes. Nebulizer therapy usually should be continued until the liquid drug volume left in the nebulizer is so low that the nebulizer ceases to function continuously and begins to "splutter". It is best to nebulize for about a minute after the 'spluttering' sound occurs, which indicates drying up of the drug solution. Tapping the nebulization chamber when the 'spluttering' begins increases the drug output.
In recent studies performed using arformoterol inhalation solution in a standard jet nebulizer, the total time for nebulization was reported as 6 minutes.
What is Residual Volume?
This is the volume of liquid drug remaining in the nebulization chamber when nebulization has ceased. It will affect the drug output from a given fill volume. If the residual volume is less than 1 ml, a fill volume of 2-2.5 ml may be adequate; nebulizers with residual volumes of more than 1 ml generally require fill volumes 4 ml.
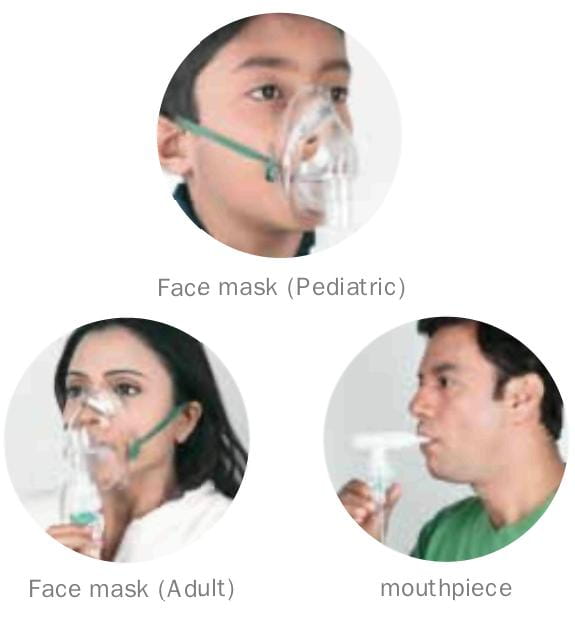
Is it Preferable to Use a Face Mask or a Mouthpiece?
Nebulizer generated aerosols can be inhaled via either a mouthpiece or a face mask. The use of a face mask with a nebulizer or spacer device has been shown to be an effective method of drug delivery for children too young to use a mouthpiece, or if the patient is sick or uncooperative. Tight fitting masks are thought to improve drug delivery. The potential problems with face masks are that some of the drug will land on the face or in the eyes or may be inhaled through the nose; also, sometimes, the mask may not fit precisely, leading to leakage of the drug.
A mouthpiece (in patients old enough to use one reliably) will increase lung deposition of the drug, compared to a face mask. Thus, the available evidence suggests that a mouthpiece is preferable to a face mask for aerosol delivery. While using the mouthpiece, the use of a nose clip is not recommended because of inconvenience and discomfort, and the lack of strong evidence to support its use.
There have been reports of ocular complications with symptoms when nebulized ipratropium has escaped into the eyes. Nebulized steroids can cause bruising, hoarseness and candidiasis of the mouth and throat (thrush) in some patients. Such patients may find it helpful to wash their face and rinse out their mouth with water after nebulization.
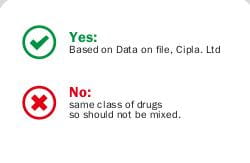
Can a Mixture of Two Different Drugs be Used for Nebulization?
Clinicians and patients prefer to mix formulations to decrease the time required for the treatment; however, care should be taken to see that the formulations mixed are compatible.
How Should the Nebulizer System be Assembled?
Qualitative Aspects of Nebulization
What are the Characteristics of a Good Nebulizer System?
The nebulizer system should deliver the maximum amount of respirable aerosol (droplets of 0.5 to 5 microns in diameter) in the minimum amount of time, with a minimum of inconvenience and wastage. Therefore, the pre-requisites of a good nebulizer system would be as below:
- Fast rate of nebulization, implying that the maximum amount of nebulized aerosol is potentially available to the patient.
- Minimum wastage of drug aerosol, implying that the maximum amount of aerosol released is delivered to the patient and not emitted into the environment.
- Low residual volume, implying that more of the fill volume will be delivered to the patient as aerosol.
- Well-defined droplet size distribution.
What are the Factors Affecting Nebulizer Performance?
Nebulizer performance depends on both the technical design of the nebulizer and on the patient using it.
Technical Factors
The performance of the nebulizer may vary as per the design. It also depends upon the following:
- Driving gas flow used
- Fill volume
- Residual volume
- Nebulization time
- Characteristics of the liquid drug (concentration, viscosity, surface tension)
Other factors may include composition of driving gas, environmental conditions, static charge, nebulizer ageing, designs to enhance nebulizer output, continuous or breath- actuated design, etc.
Usage Factors
- Tidal volume (Nose versus mouth breathing)
- Face mask or mouthpiece
- Artificial airway and mechanical ventilation
What are the Factors Affecting the Deposition of Nebulized Drugs in the Respiratory Tract?
The three main factors that determine the deposition of nebulized drug droplets in the respiratory tract are droplet size, pattern of breath inhalation and age/condition of the lungs. The lung deposition characteristics and efficacy of an aerosol depend largely on the particle or droplet size. Generally, the smaller the particle, the greater is the possibility of peripheral penetration and retention.
The velocity of air flow decreases markedly as it travels down the respiratory tract. The speed of the inhaled aerosol-laden air and its turbulent flow is greatest in the nose/mouth, pharynx, trachea and larger bronchi, and it is here that the larger particles are deposited by impaction. Within the smaller bronchi, bronchioles and alveoli, the smaller particles are removed by interception, sedimentation and diffusion.
Drug particles generated by nebulizers are often electrostatically charged. This charge may induce an equal and opposite charge on the airway wall, leading to electrostatic deposition. This mechanism is most apparent for particles less than 1 micron in diameter and for long, thin fibre-like particles.
What are the Clinically Important Characteristics of Nebulizer Performance?
Clinically important characteristics are nebulization time, cost, ease of use, and requirements for cleaning and sterilisation. Nebulization time is important for patient compliance in the outpatient setting and clinician supervision for hospitalised patients. A short nebulization time that delivers an effective dose is desirable. Many nebulizers are low-cost, mass-produced, single-patient-use devices. This results in variability in performance among the devices, which might not be important for bronchodilator delivery, but which could be important for delivery of other inhaled medications.
Care & Maintenance of Nebulizers
How Does One Ensure Good Maintenance of a Nebulizer?
Nebulizers must be cleaned regularly to avoid crystallization and the growth of microorganisms in the residual liquid in the nebulizer leading to cross infections.
Care of Nebulizer
Cleaning and disinfecting the equipment is simple, yet very important. Cleaning should be done in a dust- and smoke-free area away from open windows.
- After each treatment, rinse the nebulizer cup with warm water, shake off excess water and let it air dry.
- At the end of each day, the nebulizer cup, mask, or mouthpiece should be washed in warm, soapy water using a mild detergent, rinsed thoroughly, and allowed to air dry.
- Note: There is no need to clean the tubing that connects the nebulizer to the air compressor.
- Every third day, after washing the equipment, disinfect the equipment using a vinegar/water solution or the disinfectant solution as suggested by the manufacturer.
To use the vinegar solution, mix ½ cup white vinegar with 1 ½ cups of water. Soak the equipment for 30 minutes and rinse well under a steady stream of water. Shake off the excess water and allow to air dry on a paper towel. Always allow the equipment to completely dry before storing in a plastic, zipper storage bag.
Compressor Care
- Cover the compressor with a clean cloth when not in use. Keep it clean by wiping it with a clean, damp cloth as needed.
- Do not put the air compressor on the floor either for treatment or for storage.
- Check the air compressor's filter as directed. Replace or clean according to the directions from your equipment supplier.
- Always have an extra nebulizer cup and mask or mouthpiece in case you need it.
- Store medicines in a cool, dry place. Check them often. If they have changed color or formed crystals, throw them away and replace them with new ones.
- All equipment for the nebulizer therapy can be obtained through your equipment supplier.
Important: Unplug the compressor before cleaning it.
Methods of Nebulization
What is Home Nebulization?
The place of nebulizer therapy in the treatment of acute exacerbations of airway diseases has been validated time and again. While most patients can manage their airway diseases with MDIs or DPIs, some patients may still require regular therapy with nebulization at home. This form of treatment may be termed as 'home nebulization'.
Indications for home nebulization would include the following:
- Patients who cannot use other inhaler devices like infants, children and very elderly patients.
- Patients with chronic oral steroid dependent asthma, where the aim is to reduce the dose of oral steroids.
- COPD patients with co-morbidities like rheumatoid arthritis or cognitive disorders, who may be exhibiting a lack of ability to operate other handheld inhaler devices effectively.
- Severe airway disease patients requiring high-dose medication, which can be achieved via nebulizer therapy.
- After appropriate instruction and demonstration, the patient is judged incapable of performing the MDI manoeuver.
- Spirometry showing
- Very less inspired vital capacity OR
- Inspired flow is less than 30 L/min, OR
- Breath hold capacity is less than 4 seconds
- MDI user demonstrating recurrent episodes of acute airflow obstruction that compromises his ability to use the device.
What is Continuous Nebulization?
Continuous aerosolised bronchodilators are occasionally used in the treatment of acute asthma. A typical dose range for continuous salbutamol is 5 to 15 mg/h. The available evidence suggests that this therapy is safe and at least as effective as intermittent nebulization. Several configurations have been described for continuous nebulization, including frequent refilling of the nebulizer, use of a nebulizer and infusion pump, and use of a large-volume nebulizer.
More consistent aerosol delivery can be obtained with a small-volume nebulizer attached to an infusion pump than with a large-volume nebulizer. A commonly used large-volume nebulizer for this therapy is the High-Output Extended Aerosol Respiratory Therapy (HEART) nebulizer.
The large-volume HEART nebulizer maintains consistent output up to 8 hours and provides an acceptable method for delivering continuous aerosol through an infant ventilator circuit.
What is the Optimal Technique of Using a Nebulizer in Ventilated Patients?
- Suction endotracheal and airway secretions.
- For patients with known intolerance or chronic lung disease, consider pretreating with bronchodilator like salbutamol.
- Place the nebulizer in the inspiratory line 46 cm from the patient Y connector or 30 cms from the ET tube.
- Turn off flow-by or continuous flow during nebulizer operation.
- Remove humidifier from circuit (do not disconnect).
- Use a ventilator if it meets the nebulizer flow requirements and cycles on inspiration or use continuous flow from external source.
- Adjust ventilator volume or pressure limit to compensate for added flow.
- Ensure that, fill volume of nebulizer, time and gas flow rates are optimal.
- After completion, remove nebulizer from circuit, rinse with sterile water and dry, store in safe place.
- Reconnect humidifier, return ventilator settings and alarms to previous values.
- Use a closed circuit ventilation system with additional expiratory filter.
- Monitor patient for adverse response, if any.
Practical Points for Maximum Benefit with a Nebulizer
- Place the compressor where it can safely be plugged to a power source and where one can reach the ON/OFF switch.
- Wash hands prior to each treatment.
- Use a clean and dry nebulizer.
- Fill volume is usually 2 to 4 ml.
- Most jet nebulizers work at a flow rate of 6 to 8 L/min.
- Oxygen can be used if a compressor is not available.
- Holding the nebulizer in an upright position prevents spillage and promotes better nebulization.
- Occasionally tapping the side of the nebulizer is beneficial.
- Nebulization time for bronchodilators is generally <10 minutes.
- A pattern of steady normal breathing, combined with occasional deep breathing is beneficial.
- Respules contain liquid drugs, which are pre-diluted; hence, they can be used directly.
- The respirator solution should be diluted in a ratio of 1:3 i.e. 1 part of drug concentrate to 3 parts of normal saline (0.9% sodium chloride solution).
- Care should be taken that after diluting, the fill volume should not be in excess of 2 to 4 ml. Do not use distilled water or tap water for dilution.
- Use of combination products is preferable over mixing drugs.
- Always follow the manufacturer's recommendations for cleaning. The nebulizer should be run empty for sometime, before the next use, after cleaning.
- Any scratches, damage, or discolouration indicates that the nebulizer and the tubing should be changed.
Glossary
Aerosol: A two-phase system made up of a gaseous continuous phase (usually air) and a discontinuous phase of individual liquid or solid particles
Aerosol Output: Mass per minute of particles in aerosol form produced by the nebulizer.
Heterodisperse Aerosol/Polydisperse Serosol: Aerosol made up of particles of many different sizes
Inspiratory Flow Rate: Rate or velocity of air at which it is inhaled.
Microns (μ): Measure of geometric diameter of aerosol particle.
Monodisperse Aerosol: Aerosol particles are all the same or very nearly the same.
Rate of Nebulizaion: (Mass of drug added - mass of drug remaining) Nebulization time
Residual Volume: Volume of liquid remaining in the nebulizer reservoir when nebulization has ceased
Respirable Practicles: Particles <5 microns in aerodynamic diameter.
Respirable Fraction: Proportion of respirable particles in the aerosol output expressed as a percentage.
Respirable Output: Mass of respirable particles produced per minute (aerosol output - respirable fraction)
Tidal Breathing: Normal steady breathing.
Tidal Volume: Volume of air that enters and leaves the lungs during normal breathing (500 ml).
Ultrasonic: Pertaining to sound frequencies so high (greater than 20 kilohertz), the human ear cannot perceive them.
Venturi: A short tube with a constricted throat used to determine liquid pressures and velocities by measurement of differential pressures generated at the throat as a liquid traverses the tube.
Viscosity: The material property that measures a liquid's resistance to flowing.
References
1. Practical Handbook of Nebulizer Therapy. Martin Dunitz; an imprint of Taylor & Francis Group. London,
UK.
2. Drugs 2007; 67: 903-14. Aerosolised antibacterials for the prevention and treatment of hospital-acquired
pneumonia.
3. Eur Respir J 2001; 18: 228-42. European Respiratory Society Guidelines on the use of nebulizers.
4. Thorax 1997; 52 (Suppl 2): S1-106. Current best practice for nebulizer treatment. The Nebulizer Project
Group of the British Thoracic Society Standards of Care Committee.
5. Pharm World Sci 2000; 22: 75-81. A review of the technical aspects of drug nebulization.
6. Respir Care 2000; 45: 609-22. Nebulizers: Principles and performance.
7. Respir Care 2002; 47: 1290-301; discussion 1301-4. Review. Assessing nebulizer performance.
8. Respir Care 2004; 49: 174-9. Performance comparison of nebulizer designs: Constant output,
breath-enhanced, and dosimetric.
9. Respir Care 2007; 52: 866-84.The role of aerosolized antimicrobials in the treatment of ventilator-associated
pneumonia.
10. Respir Care 2008; 53: 699-723; discussion 723-5. Aerosol delivery devices in the treatment of
asthma.
11. Journal of Cystic Fibrosis 2006; 5: 205-213 Inhalation solutions - which ones are allowed to be
mixed? Physicochemical compatibility of drug solutions in nebulizers.
12. Surg Infect (Larchmt) 2007; 8: 73-82. Aerosolized tobramycin in the treatment of ventilator-associated
pneumonia: a pilot study.