Are You Prescribing the Correct Inhalation Device?
Introduction
Inhalation is the preferred route of drug delivery for obstructive airway diseases (OADs) such as asthma and chronic obstructive pulmonary disease (COPD) as it allows delivery of smaller doses of the medication directly to the target site of action, resulting in fewer systemic side-effects. A successful pulmonary administration requires a harmonic interaction between the drug formulation, the inhaler device, and the patient. Appropriate selection and correct use of inhalation devices is an integral component in the management of respiratory diseases.
There are many challenges with the use of inhalers like difficulties related to lung disease severity and pulmonary function, physical considerations, including manual dexterity and comorbidities such as arthritis. In terms of device selection and adherence, patient engagement and satisfaction are also important factors to consider.
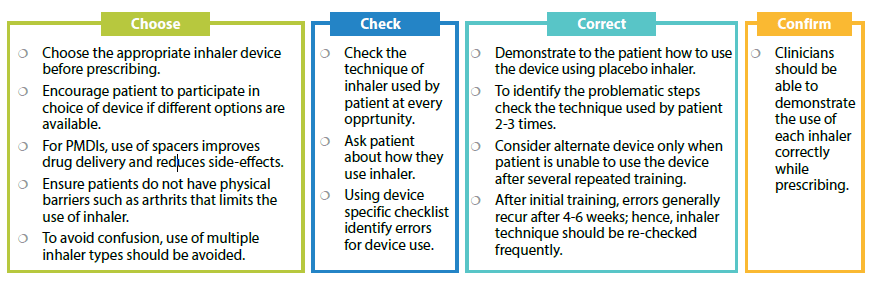
Non-adherence and poor inhaler technique are the most important concerns in the management of patients with asthma and COPD. The correct use of inhaler devices, along with adequate training and monitoring of the patient’s inhalation technique are the important aspects to be considered while treating.
Types of Inhalation Devices
Inhaler devices vary in several ways, including how the inhaler dispenses the medication, whether the treatment is passively or actively generated (e.g., using propellant, mechanical, or compressed air), aspects of the drug formulation (e.g., solution, dry powder, or mist), whether the inhaler contains medication in a single- or multi-dose, and whether the device is disposable or refillable.
The most commonly used devices include pMDIs, DPIs, and the nebulizers.
Pressurized Metered Dose Inhalers (PMDIs)
A general pMDI is a portable, compact and multidose device, which is quick and easy to use, suitable for emergencies and the dose available for inhalation and particle size is independent of inhalation manoeuvre.
However, for optimal drug delivery, co-ordination between inspiration and actuation is necessary. It needs to be shaken before each inhalation and primed if not used within a specific time. It is not suitable for young children (without use of spacer) and chances of oropharyngeal deposition of particles are higher.
Common user errors with pMDIs include inhaling too fast (and thus not slowly and deeply), failure to empty lungs prior to inhalation, and failure to hold breath following inhalation.
Dry Powder Inhalers (DPIs)
DPIs are small and portable, breath-actuated inhalation devices which do not require hand-breath co-ordination and can be used for most medications. They can be single or multiple-dose devices. In single dose devices, patient can confirm whether the medication has been correctly taken by checking the capsule remnants.
However, DPIs are not suitable for emergencies, not suitable in very young children, and require sufficient inspiratory flow for optimal drug inhalation. Each new dose needs to be inserted in single-dose DPIs and Patient must continue or repeat inhalation until capsule is empty. They are also sensitive to humidity and require more care for maintenance.
Common errors with DPIs include not keeping the device in the correct position while loading the dose, failure to tilt head in the correct position, insufficient inspiratory effort, and not emptying lungs before inhalation.
|
Devices |
Advantages |
Limitations |
|
PMDIs |
|
|
|
DPIs |
|
|
Nebulizers
Nebulizers are mostly used in the emergency setting for the acute treatment of patients, or in chronic disease management for children or elderly patients who are unable to use an inhaler with a spacer or who have coordination problems. As nebulizers omit the need for patient coordination between inhalation and actuation, these devices are particularly useful in those with cognitive, neuromuscular, or ventilation impairments. As nebulizers provide a large dose with very little patient coordination skill, and allow for concomitant oxygen delivery, they are highly useful in treatment of severe exacerbations of respiratory disease.
However, most nebulizer devices are bulky and inconvenient, require regular maintenance, prolong drug delivery from seconds to 10–15 minutes, and require regular thorough cleaning to sterilize the device. To overcome the limitation, newer devices are now developed which are hand-held and portable.
Inhaler Selection in Clinical Practice
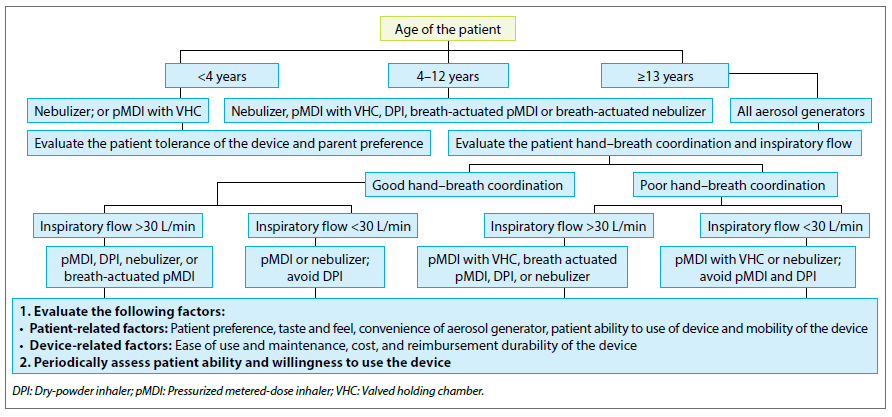
Choice of inhaler depends on a combination of factors including pulmonary function (ie inspiratory flow and breathing technique), device handling, use of a spacer, required inhaler technique, and patient preference.
Many factors come into play while choosing the appropriate device for the patient.
Age of the patient: Young children and elderly population may lack the necessary hand-breath coordination required in using PMDIs.
Peak Inspiratory flow rate (PIFR): Drug delivery is dependent of PIFR when using DPIs. Children and elderly population or those with severely impacted PIFR (<30L/min) should not be prescribed DPIs.
Severity of lung disease: In severe lung diseases mucus plugging, and increased airway obstruction can impair deposition of the drug in the lung periphery. In COPD patients, inspiratory flow rates may be decreased by severe expiratory airflow limitation, decreased inspiratory capacity, and hyperinflation. Nebulizers and pMDI + spacers may be preferred in such conditions.
Physical and cognitive ability of the patient: A certain amount of dexterity and timing is required for correct usage of aerosol devices. Limitations in the elderly population such as arthritis, tremors, incoordination, stroke, muscle weakness, cognitive impairments must be taken into account while selecting the correct inhalation device.
Patient Factors: Patients may exhibit preference to certain devices based on portability and compact design of the device, as well as noise, taste, treatment time, and convenience
Cost: Lower socio-economic status affects adherence to therapy. The inhalation device prescribed should be at an affordable cost to the patient.
Screening Guidelines for Device Selection
- For children less than 4 years, choose Nebulizer or pMDI with Valve Holding Chamber (VHC) and facemask
- For kids in age group 4-12 years, go for breath actuated pMDI or breath actuated DPI. Nebulizer and pMDI with VHC are other alternatives.
- For patient population greater than 13 years, evaluate the hand-breath coordination and PIFR. DPIs should be avoided if PIFR is <30L/min and pMDIs should be avoided if the hand-breath coordination is poor.
Strategies for Effective Use of Inhalation Device: Recommendations From GINA
Conclusion
Success of asthma/COPD management highly depends on correct inhalation technique. Choosing the device after considering the various factors will help improving patient adherence to treatment and increase the success of overall disease management.
References
- Therapeutics and Clinical Risk Management 2019:15 461–472
- Med Devices (Auckl). 2015; 8:131–39.
- Expert Rev Respir Med. 2011; 5(4):561-72.
- [Respir Care 2011;56(9):1411–1421. © 2011 Daedalus Enterprises
- 2017 GINA Report.
- Respir Med. 2017; 124:6–14.
- Adv Ther. 2015; 32(4):285-92.
- Clinical Asthma 2008, Pages 303-312