Asthma: Answers to Clinical Questions (Volume 2)
Treatment of Asthma
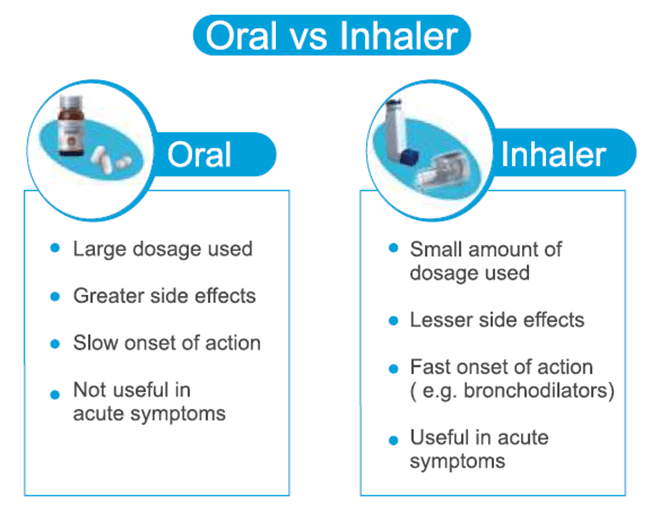
1. Why should inhalation therapy be selected over orals for treating asthma?
Inhalation therapy is the most important, most easy and effective treatment option available for asthma.
Oral medicines are have slow onset (more than 30 mins), more side effects and cannot be used during asthma attacks. On the other hand, inhalers have rapid onset (within 5 mins), minimal side effects and can be effectively used during asthma attacks.
Further the dose used in inhaler are very small (mcg) as compared to orals (mg). Very small dose is required for the desired effect in inhalation therapy.
Asthma guidelines such as GINA (Global Initiative for Asthma) also recommend the use of inhalation therapy over oral.
Thus there is no substitute for the inhalation therapy since it is the best, cheap, fast, efficacious and safe.
International Journal of Applied Pharmaceutics 2013; 5(3): 7-10
Eur Respir J 2011; 37: 1308–1331
2. Are inhaled steroids harmful?
Inhaled steroids (ICS) are age-old medicines and are absolutely safe. ICS are safe in children, pregnant women and athletes.
The steroid medicines used in inhalers for treating asthma are not the same as those used by bodybuilders and athletics. The bodybuilders take the anabolic (tissue-building) steroids which are basically synthetic testosterone while the steroids used in the inhaler are glucocorticoids which are similar to those our body naturally produces. These glucocorticoids are very important in preventing the inflammation that causes asthma. Further, the amount of steroids present in the inhaler is very small (dose is in microgram). Such minute amount of steroid in the inhaler has minimal side effects.
Pediatr Pulmonol. 2002; 33(3): 208-20
J Natl Med Assoc. 2006; 98(6): 851–861
3. Does ICS causes growth retardation in children?
No, ICS does not cause growth retardation in children when used in the recommended doses.
In randomized controlled clinical trials, the use of inhaled beclomethasone, budesonide and fluticasone was associated with a reduced growth during the first months of therapy, in the order of magnitude of approximately 0.5–1.5?cm/yr. It is, however, unlikely that such an effect continues or persists because accumulating evidence shows that asthmatic children, even when they have been treated with ICS for years, attain normal adult height.
In the longest study published till date on the safety of ICS in children, it was seen that children (aged 3–13 years) reached their final expected height even after an average of 9.2 years of long-term treatment with inhaled budesonide.
Individual rare cases have been reported, however, where ICS use was associated with clinically relevant growth suppression. It is also important to know that uncontrolled asthma itself can result in the growth retardation of the child. It has been realized that it is unwise to withhold steroids in children for fear of causing growth retardation in them.
Eur Respir J 2001; 17: 287- 294
Ugeskr Laeger. 2001; 163(48): 6746-50
4. Why should a doctor prescribe controller medicine even if a patient is satisfied on reliever medication?
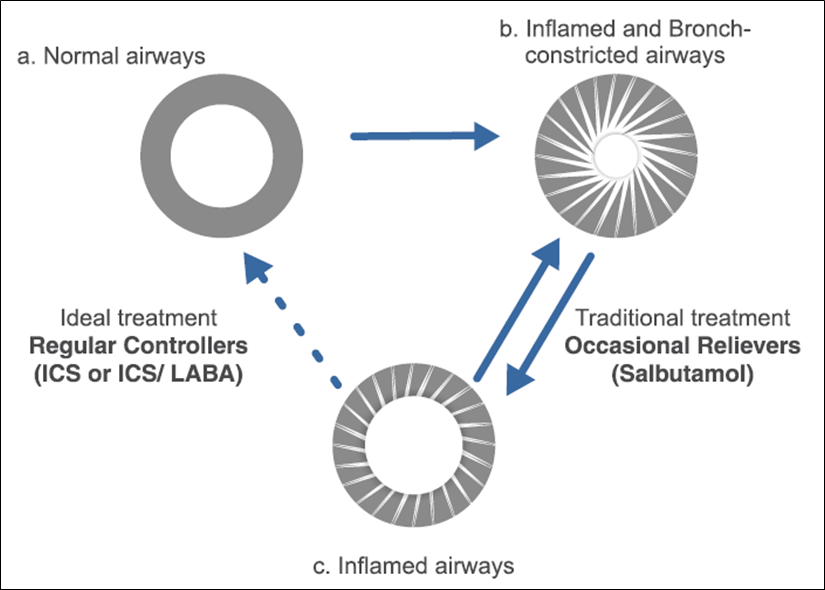
There are two components involved in asthma – Bronchospasm and Inflammation. Bronchospasm is the sudden constriction of smooth muscles which results into narrowing of airways. Inflammation is the reddening and swelling of the epithelial layer which further results into narrowing of the airways and also increases the airway hyper-responsiveness. So to treat asthma, one needs to treat both these components i.e. bronchospasm as well as inflammation.
A reliever medicine containing either salbutamol or levosalbutamol can be used to treat broncho-constriction in the airways. Relievers (salbutamol) should be taken only during asthma attacks or when patients feel breathless. Remember, an excess use of reliever medication indicates worsening of asthma. So when taken during attack, it will treat the bronchospasm. If the patient continues the treatment only with reliever, the inflammation in the airway will not be treated and the patient will just shuttle between type b. and type c. airways (see figure). Thus it temporarily treats bronchospasm but does not have any effect on inflammation which is the most important component involved in asthma.
Hence the controller become very important. A controller medicine contains either steroid (ICS) or a combination of ICS+LABA. It is very important to prescribe controller, because these medications will act on underlying inflammation and also reduce to need of relievers.
So to achieve asthma control, a doctor has to prescribe a controller (ICS or ICS/LABA) along with the relievers (salbutamol or levosalbutamol). Controller medication should be taken regularly (everyday). These controller medications will treat the inflammation, improve symptoms and improve asthma control. Remember patients might not perceive the immediate effects of controller medications because these are not rapid acting as reliever. But still one has to continue taking it, to achieve controlled asthma.
5. When should anti-inflammatory controller therapy be started?
Controller therapy (inhaled steroids) should be used in all the severities of asthma including mild persistent asthmatics. ICSs are the recommended first-line therapy for persistent asthma of all severities.
Further increased use of reliever medication (salbutamol) indicates worsening of asthma and should be treated with a controller therapy.
Cleveland and Clinic Journal of Medicine 2010; 77(6): 364-368
Global Initiative for Asthma (GINA), 2015
6. Should treatment for asthma be started with ICS or ICS+LABA?
Plain steroid (ICS) is generally preferred in very mild asthma cases. If the patient does not responds to plain ICS or if the severity of disease increases, then ICS+LABA should be given.
However the treatment in persistent asthmatics can also be started with ICS+LABA. Whenever the combination is given, the ICS acts on the inflammation while the LABA acts on the bronchoconstriction thus taking care of both the components involved in asthma. Various research studies have shown the effectiveness of ICS/LABA combination over ICS.
Global Initiative for Asthma (GINA), 2015
Pediatric Pulmonology 2009; 44: 1132–1142
7. Should ICS+LABA treatment be preferred over ICS+Montelukast?
ICS+LABA is the most important treatment for asthma since it treats inflammation as well as bronchoconstriction.
Leukotriene receptor antagonists like montelukast is an add-on therapy as they inhibit leukotrienes which are one of the important inflammatory mediator.
However ICS inhibits all the inflammatory mediators. Hence ICS+LABA should be preferred while montelukast can be added as an add-on therapy. Studies have shown that a combination of ICS+LABA produces significantly greater improvements in lung function and asthma control than the addition of montelukast to inhaled steroid.
Leukotriene modifiers used as add-on therapy may improve asthma control in patients with moderate to severe asthma.
Leukotriene modifiers may be indicated in mild asthma as an alternative to inhaled corticosteroids, or as a supplement to inhaled corticosteroids.
Respir Med. 2003; 97(3): 234-41
Respiratory Research 2007; 8: 67 (doi:10.1186/1465-9921-8-67)
8. How long ICS or ICS/LABA should be given to patients?
Asthma is a chronic disease. However it can be controlled with appropriate medicines and appropriate use of inhalation devices.
Ideally if the patient continue to experience symptoms (breathlessness, cough, wheezing, chest tightness), treatment should be continued. The dose can be increased (usually called as step-up) if symptoms or severity increase and if patient has one or more exacerbation risk factor.
On the other hand, if symptoms decrease over the period of time and patient feels better, the doctor can reduce the dose (step-down). Guideline recommend to step down treatment if symptoms are controlled for 3 months and patient has low risk factors for exacerbations.
Sometimes after the treatment if the patient is completely controlled for 6-12 months, and has no risk factors, the controller medications (ICS or ICS/LABA), can be stopped; however the patient has to be regularly monitored. The patient still have to take reliever medication (salbutamol or levosalbutamol) if he/she experience any breathlessness.
Complete cessation of ICS in adults is not advised as the risk of exacerbations increases.
Global Initiative for Asthma (GINA), 2015
9. Which ICS/LABA combination should be preferred?
There are several ICS/LABA combination available such as:
- Salmeterol / Fluticasone
- Formoterol / Budesonide
- Formoterol / Fluticasone
- Formoterol / Beclomethasone
- Formoterol / Mometasone
There are differences in the pharmacokinetics and dynamics properties of individual molecules. But overall, all the available ICS/LABA combinations have similar efficacy. The selection of a particular combination may be based upon the dose, age group recommendation, cost etc.
10. Which ICS/LABA has the most favorable safety profile?
All the ICS/LABAs such as salmeterol/fluticasone, formoterol/budesonide, formoterol/beclomethsone, formoterol/mometasone, and formoterol/ciclesonide have equivalent safety profile.
11. When should oral corticosteroids be used? Do they have any side effects?
Short-term oral corticosteroid therapy is required in the treatment of severe acute exacerbations because they prevent progression of the asthma exacerbation, reduce the need for referral to emergency departments and hospitalization, prevent early relapse after emergency treatment, and reduce the morbidity of the illness.
Long-term oral corticosteroid therapy (that is, for periods longer than two weeks as a corticosteroid “burst”) may be required for severely uncontrolled asthma, but its use is limited by the risk of significant adverse effects. If oral glucocorticosteroids have to be administered on a long-term basis, attention must be paid to measures that minimize the systemic side effects. Guidelines recommend that approximately 30 mg/day (or 1 mg/kg/day) of prednisolone may be given until 2 days after full recovery and stopped or tapered thereafter (5-7 days).
Systemic corticosteroids are known to cause a number of side effects when taken over a long period. The reported adverse events are osteoporosis, cataract, growth retardation in children, skin atrophy, acne, suppression of HPA axis, aseptic bone necrosis, hyperlipidemia, diabetes, hypertension etc.
Eur Respir J 2007; 30: 1035–1037
Respiratory Medicine 2004; 98: 275–284
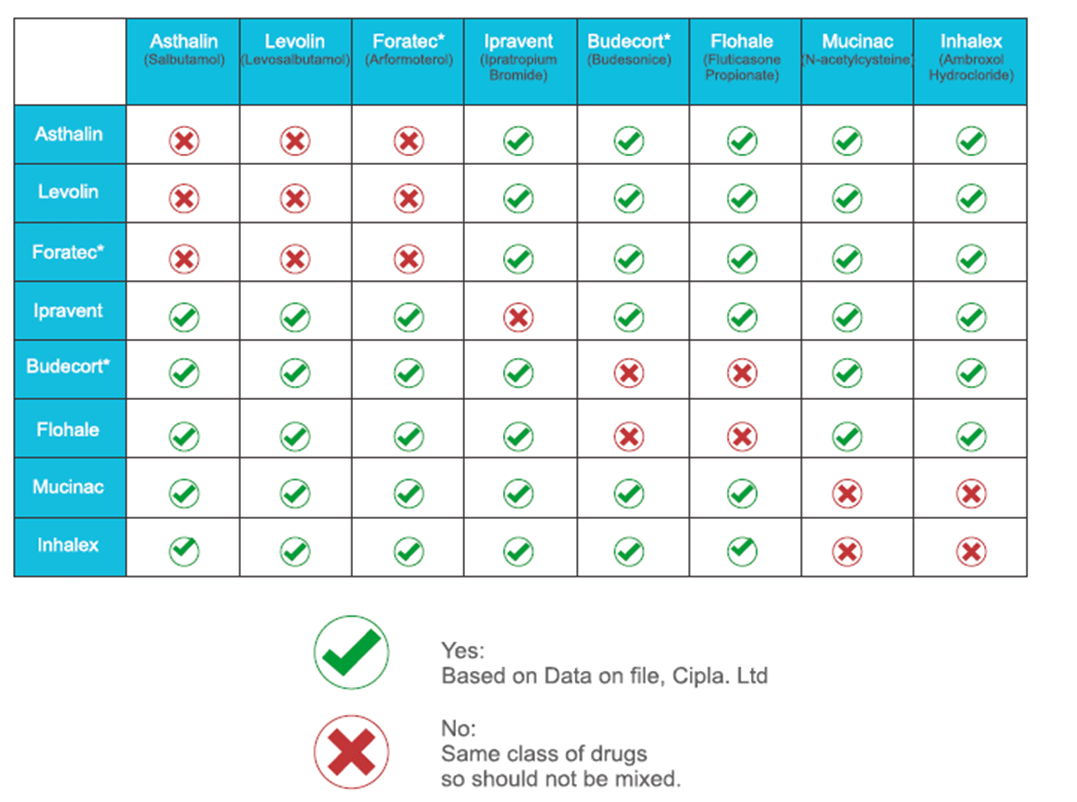
12. Can we mix different drugs in a nebulizer?
Clinicians and patients prefer to mix formulations to decrease the time required for the treatment; however, care should be taken to see that the formulations mixed are compatible. Respules available in India are fluticasone, budesonide, arformoterol and a combination of formoterol/budesonide.
13. Which is the preferred steroids to be used in acute asthma?
Of the currently available ICS, only nebulized fluticasone is indicated for acute asthma in age group of 4-16 years. Budesonide in combination with formoterol in Metered Dose Inhaler (MDI) and Dry Powder Inhaler (DPI) is used as a Single Maintenance and Reliever Therapy (SMART) in adults, 18 years and above.
For adults, systemic steroids are recommended along with bronchodilators. Eg: Oral steroids – Prednisolone, I.V. steroids – Methyl prednisone, Hydrocortisone.
14. Can inhalers be given to seasonal asthmatics for 5-6 months only?
Inhalers can be given for seasonal asthmatics for a period of 5-6 months, but still it would be beneficial to continue the medicine throughout the year in order to achieve better control of asthma.
Once the control is achieved and patient feels better, the doctor can then think of reducing the dose (step down) or can also stop the medicine if patient was already on lowest dose.
J Allergy Clin Immunol 2009; 124: 1197-203
15. Should a small child taking inhaled steroid need to take it all his/her life?
40% of girls and 50% of boys outgrow asthma after puberty. In such individuals, there is no need to take medicines. However if person experience symptoms of asthma, then yes, the medications should be restarted and continued till the time, asthma is totally controlled.
16. Are there different asthma medicines for children below 5 years and also are these medications safe in children?
The medications used in children below 5 years is somewhat similar to those used in the treatment of adults. The treatment can be started with a low dose daily or intermittent ICS or with a LTRA. If the child is not well-controlled, ICS dose can be doubled or LTRA can be used as an add-on to low dose ICS. Further an SABA should be used whenever there is an asthma attack.
17. What precautions and treatments should be taken for managing asthma in pregnancy?
Asthma is the most common chronic pulmonary disease that complicates approximately 4% of all pregnancies. Asthma may begin or be diagnosed during pregnancy, or the severity of asthma may change in association with pregnancy. Adequate pulmonary function during pregnancy is critical. Studies have shown that inadequately controlled asthma may have an adverse outcome on the foetus due to foetal hypoxia. Therefore, pregnant asthma patients must continue to take their medications.
The aims and principles of treatment are the same as in the non-pregnant patient, and asthma should be treated as aggressively in pregnant women as in non-pregnant women. Appropriately monitored use of inhaled corticosteroids, ß2-agonists and leukotriene modifiers (specifically, montelukast) are not associated with an increased incidence of foetal abnormalities. Inhaled corticosteroids have been shown to prevent exacerbations of asthma during pregnancy. Most of the evidence is available with inhaled budesonide. Acute exacerbations should be treated aggressively in order to avoid foetal hypoxia. Treatment should include nebulised rapid-acting ß2-agonists and oxygen and systemic corticosteroids should be instituted when necessary. For most medications used to treat asthma, there is little evidence to suggest an increased risk to the foetus. Pregnant patients with asthma should be advised that the greater risk to their baby lies with poorly controlled asthma.
Managing Asthma During Pregnancy: Recommendations for Pharmacologic Treatment – Updated 2004, National Institutes of Health, National Heart, Lung, and Blood Institute (http://www.nhlbi.nih.gov/health/prof/lung/asthma/astpreg/astpreg_qr.pdf)
PLoS One. 2013; 8(4): e60247 (doi: 10.1371/journal.pone.0060247)
18. Asthma medicine fall in which pregnancy category?
|
Category B: Animal studies have shown an adverse effect, but adequate and well-controlled studies in pregnant women have failed to demonstrate a risk to the fetus in any trimester. Category C: Animal reproduction studies have shown an adverse effect on the fetus and there are no adequate and well-controlled studies in humans, but potential benefits may warrant use of the drug in pregnant women despite potential risks. |
All asthma medication (ICS, LABA, SABA) fall in category C except budesonide, montelukast and zafirlukast which fall in category B.
19. Can inhaled steroids be given to diabetics?
There have been very rare reports of increases in blood glucose levels in patients with or without a history of diabetes mellitus. This should be considered in particular when prescribing to patients with a history of diabetes mellitus.
20. What is immunotherapy and when it should be used?
Immunotherapy by the use of an allergen injection was introduced in the early twentieth century. In North America, it was the treatment of choice for allergic rhinitis and asthma. In the United Kingdom, however, it was never widely used, perhaps due to the availability of selective ?2-agonists and inhaled steroids 15 years before they could be prescribed in the United States. Appropriate immunotherapy requires identification and use of single well-defined clinically relevant allergen. However, due to multiplicity of allergens and potential for serious side effects, the role of specific immunotherapy in asthma is limited. Because many asthma patients react to multiple factors that are ubiquitous in the environment, avoiding these factors completely is usually impractical. Also, due to certain limitations of immunotherapy, pharmacotherapy remains an important role to maintain good asthma control.
According to GINA guideline, the efficacy of allergen immunotherapy in asthma is limited. Compared to pharmacological and avoidance options, potential benefits of allergen immunotherapy must be weighed against the risk of adverse effects and the inconvenience and cost of the prolonged course of therapy.
Global Initiative for Asthma (GINA), 2014