Breathe-O Meter
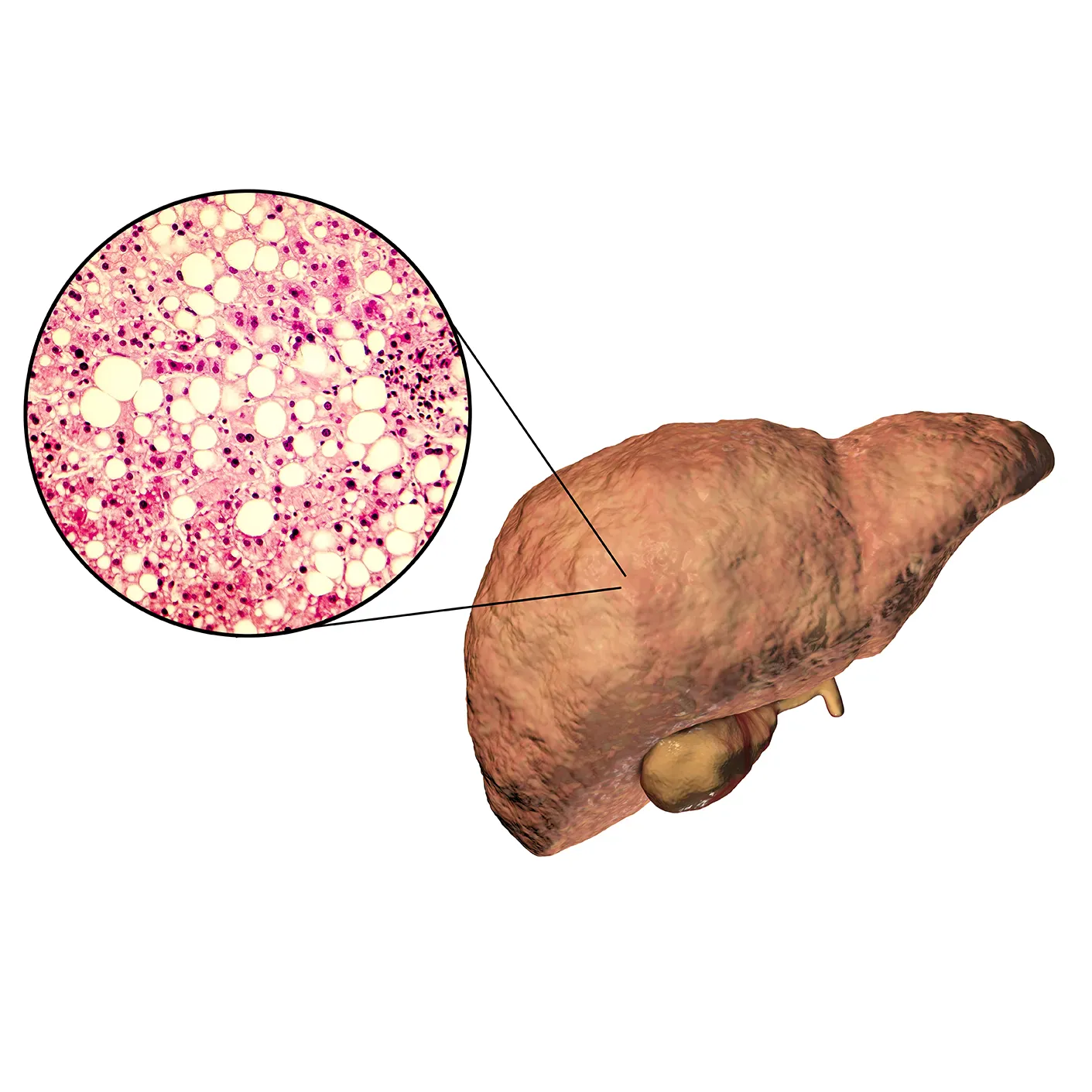
Asthma is a chronic inflammatory disease of the airways characterized by airflow limitation. Airflow limitation can be measured by spirometry or by using a simple, handy and easy to use device called the peak flow meter.
In clinical practice, inadequate usage of objective tools such as the spirometer and peak flow meter results in under diagnosis of obstructive airway diseases. In addition, many asthma patients may have poor recognition of their symptoms. Studies have also shown that symptoms may not correlate with the severity of asthma. Hence, merely relying on symptoms like cough, breathlessness and wheeze can be misleading at times.
In other diseases such as hypertension and diabetes, the use of handy tools such as the sphygmomanometer and glucometer has revolutionized disease management. Another simple example is that of a thermometer, which measures the body temperature and is used for detecting the severity of fever and also to see if antipyretics are working. Similarly, a very simple to use and portable device called the peak flow meter, which provides an objective measure of the lung function in terms of the peak expiratory flow rate (PEFR), is an important tool in the management of asthma. Various guidelines, including the Global Initiative for Asthma (GINA) have established its role in confirming the diagnosis and assessing the severity of asthma, thereby enabling proper management and improving patient compliance to the treatment prescriptions, which will also encourage adherence to asthma therapy. However, although the peak flow meter is a key tool for respiratory practice, it is not being widely used in India.
The new breathe-o meter is a peak flow meter made by Cipla, using the European Union Scale. It has been developed to provide practitioners in India with a powerful tool in diagnosing and monitoring their patients with asthma.

PEFR is the maximum flow of air that can be generated during forceful expiration after taking a complete deep breath. The PEFR represents the calibre of the large airways, i.e., it is reduced when there is obstruction in the large airways, which typically happens in asthma and advanced chronic obstructive pulmonary disease (COPD).
The PEFR can be measured by a peak flow meter such as the breathe-o meter. The peak flow meter is a simple, portable, easy-to-use, cost-effective instrument that measures the PEFR.
The PEFR can also be measured by a more sophisticated instrument such asa spirometer.
The PEFR values are majorly determined by the following:
- Patency of airways
- Patient demographic factors like race, age, height and gender of the patient
- Patient cooperation and effort
- Neuromuscular coordination
- Malnutrition
- Environmental effects
Obstruction of the large airways due to inflammation of the airways, leading to airway thickening, smooth muscle contraction and airway remodelling, is a characteristic feature of asthma. Hence, asthma patients have a reduced PEFR (reduced to less than 80% of the predicted PEFR value, suggesting a marker of asthma severity) and this is proportional to the severity of asthma, which can increase by more than 60 L/min or 20% on administration of a short-acting bronchodilator. Inhaling a short-acting bronchodilator often increases the PEFR reading.
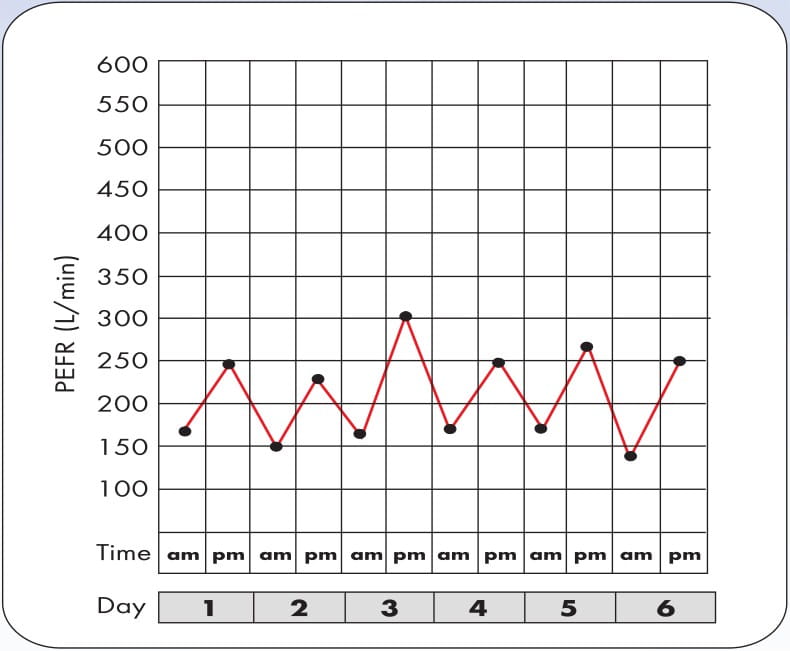
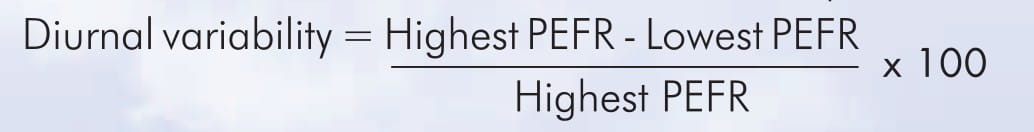
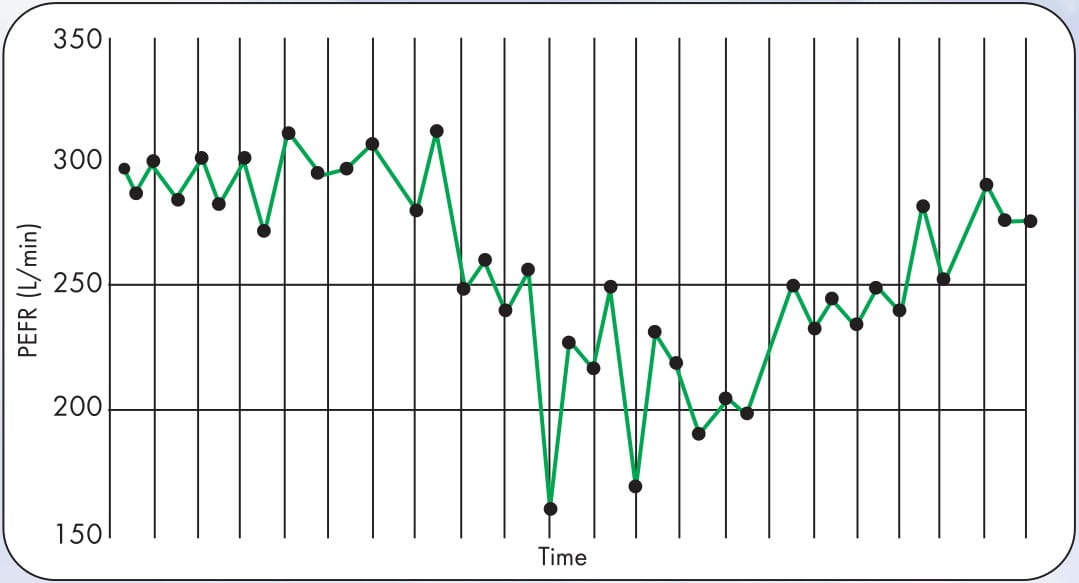
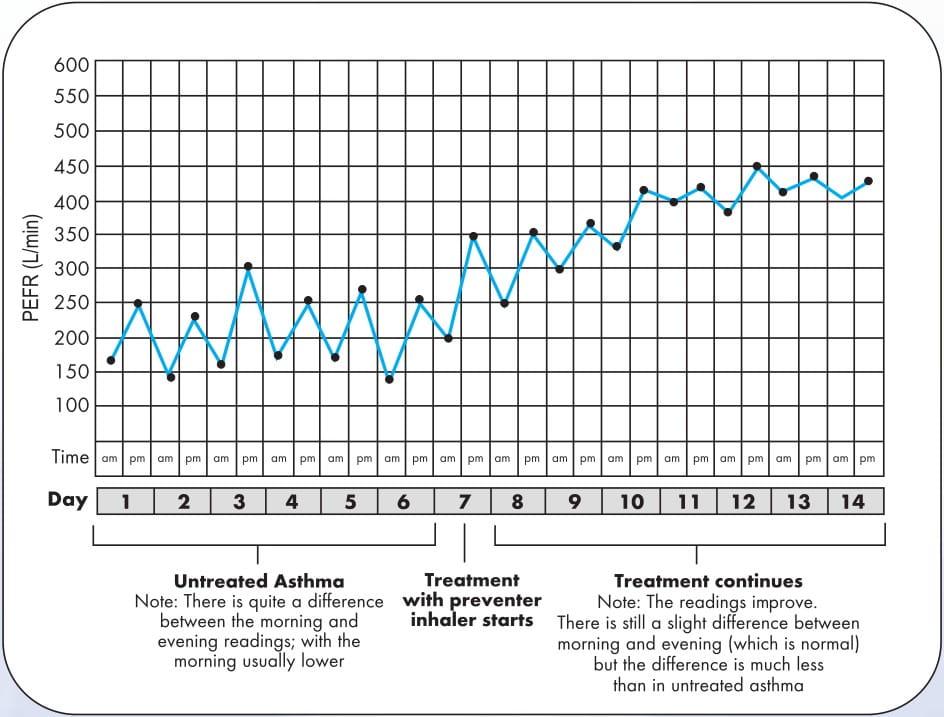
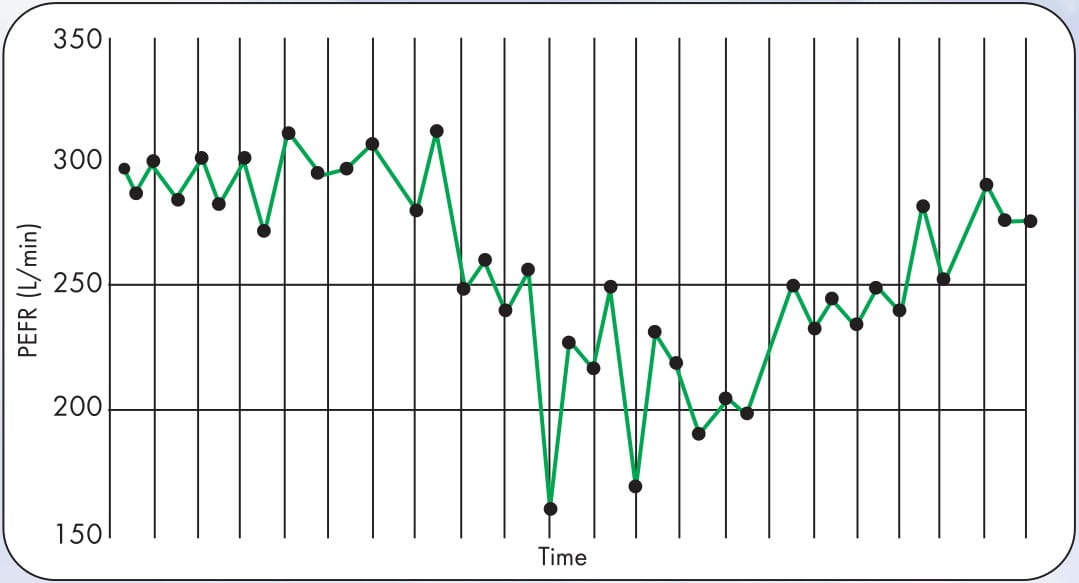
A variation in the PEFR during the course of the day is commonly observed in patients with asthma (Fig.1). Variability of the PEFR decreases with better asthma control.
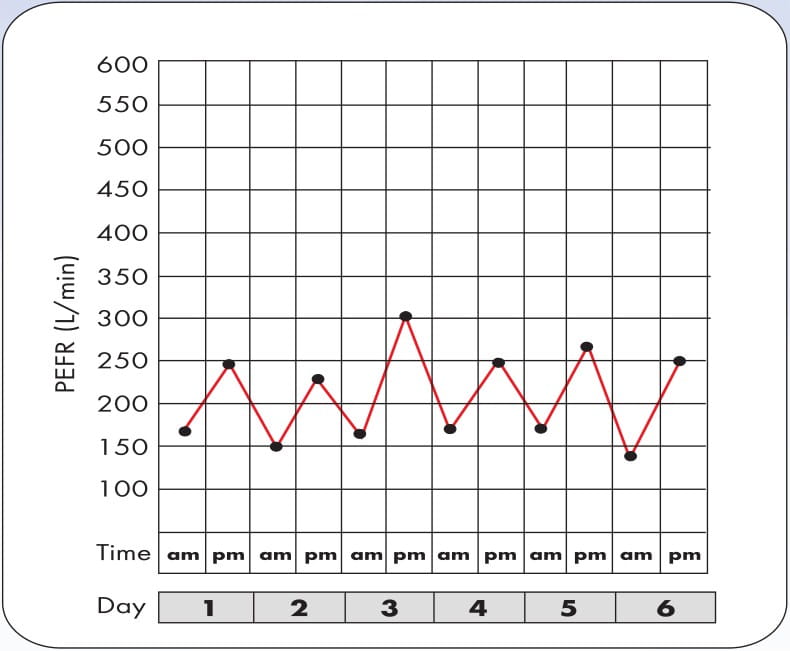
The PEFR is usually lower in the morning and higher in the evening in all individuals. This is called diurnal variability. Asthma can also be diagnosed by using the diurnal variability, which is abnormally high in asthma patients. A diurnal variability of more than 20% strongly suggests a diagnosis of asthma. For diagnosing asthma, the diurnal variability has to be measured for 14 days. The PEFR is to be measured daily in the morning (best of three readings) and evening, and the variability of each day is to be calculated by the formula mentioned below and then, the variability is to be averaged for 14 days.
The difference between the highest and the lowest PEFR, expressed as a percent of the highest PEFR, is termed as diurnal PEFR variability. An asthmatic's peak flow graph shows wide fluctuations, giving it a "saw-toothed" appearance. The wider the fluctuation, the more severe is the asthma. Diurnal variaton in the PEFR is expressed as-
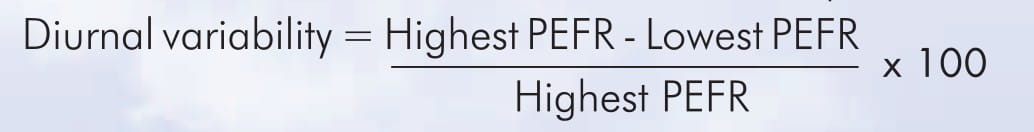
Diurnal variability >20% suggests a diagnosis of asthma.
The normal expected PEFR for a person is called as his/her predicted PEFR. It is dependent on the race, height, age and gender of the individual. The predicted PEFRs for the Indian population are now available and can be found by just looking up the PEFR respective to the gender, height and age of the individual in a predicted PEFR chart developed by the Chest Research Foundation (CRF), India. The normal predicted PEFR values lie between 350 and 650 L/min.
Since the PEFR is dependent on various factors, some people may prefer using the personal best PEFR value rather than the predicted "normal" PEFR value. The personal best is the highest PEFR measurement achieved when the patient's asthma is under control and is free of symptoms.
In the absence of the availability of predicted values for the PEFR, the "personal best" could be used as a marker for assessing the lung function of an asthma patient. An asthma patient can be treated with inhaled steroids and bronchodilators and his/her PEFR can be evaluated for a period of 2 to 3 weeks. The maximum PEFR value obtained during this asymptomatic period can be regarded as the patient's personal best. The PEFR measured during the follow-up visit can be compared with the personal best for that patient, which gives a fair judgment about improvement or worsening of asthma.
Some patients are poor perceivers of their symptoms and miss early detection of their exacerbations and land up with acute severe exacerbation in hospital. Home monitoring in such patients could be life-saving. Many patients may want to monitor their asthma at home, but it must be the preferred course in the following patients:
- High-rks patients (e.g., those with previous life threatening asthma)
- Unstable asthma (e.g., following hospitalization or after changing medications)
- Patients with unreliable or relatively insensitive perceptions of airflow obstruction (poor preceivers).
Home monitoring with a peak flow meter improves days lost from work, acute exacerbations, increases the FEV1 and mean PEFR, and also reduces the use of inhaled ?2 agonist rescue medication.
PEFR home monitoring (on recommendation by the doctor) PEFR readings should be recorded twice daily, first thing in the morning and then at bedtime. Diary cards, which will provide a graphical record of the PEFR trends, should be maintained. These PEFR patterns help the doctor make an asthma management plan, which enables the patient to make treatment decisions at home and indicates when he/she should seek emergency help.
The duration of PEFR home monitoring will vary, depending on the patient's clinical condition. Long-term daily monitoring should be undertaken in patients with more severe/unstable asthma.
The PEFR, during an acute exacerbation, helps to judge the response to the prescribed medications and the severity of airflow obstruction.
Admission to hospital is a valuable opportunity to introduce or review the PEFR monitoring and formulate an asthma action plan. However, PEFR monitoring in the hospital is not a substitute for performing spirometry at discharge or at follow-up.
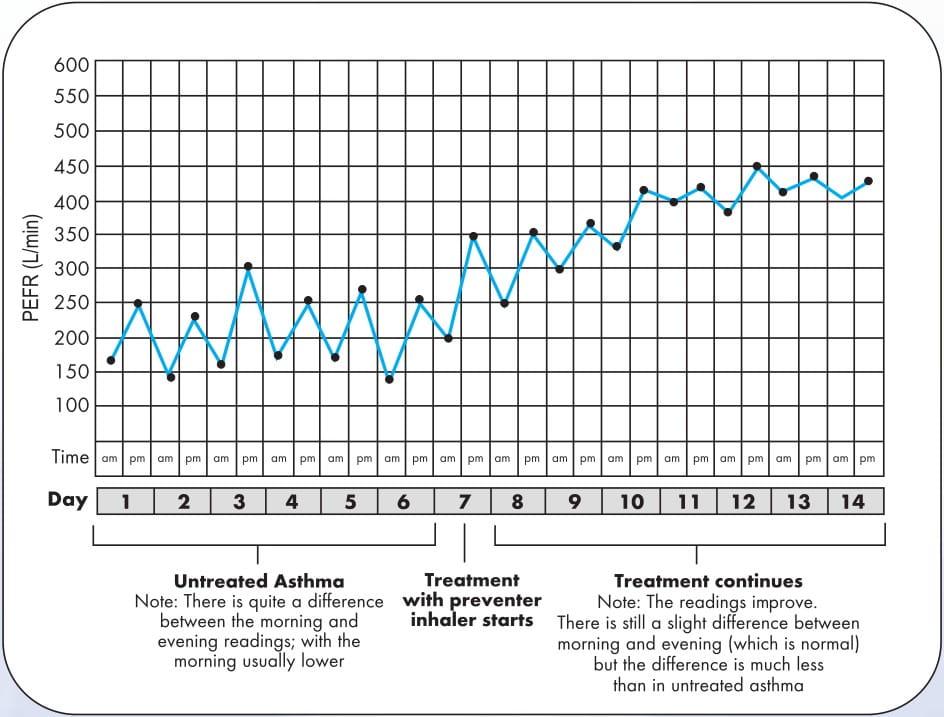
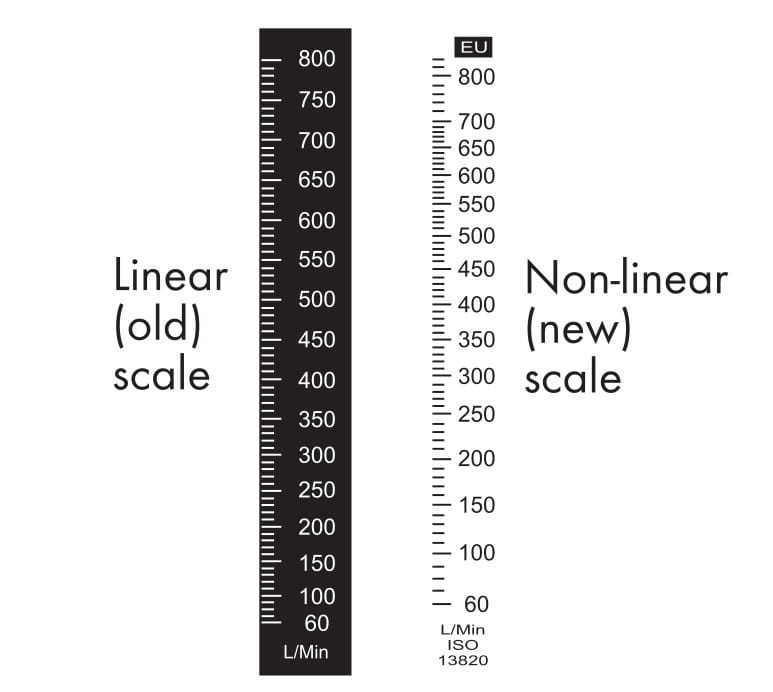
A number of peak flow meters are available and are currently in use. However, there may be significant differences between them because of non-linearity. Studies have revealed that the linear scales on the peak flow meters overestimate the PEFR in the low-to mid-range on the scale and underestimate PEFR values in the high range on the scale, when compared with highly sensitive and accurate flow measuring techniques. Accordingly, the breathe-o meter has a new log-linear scale and conforms with the EN 13826:2003 standards thereby improving the accuracy of the breathe-o meter
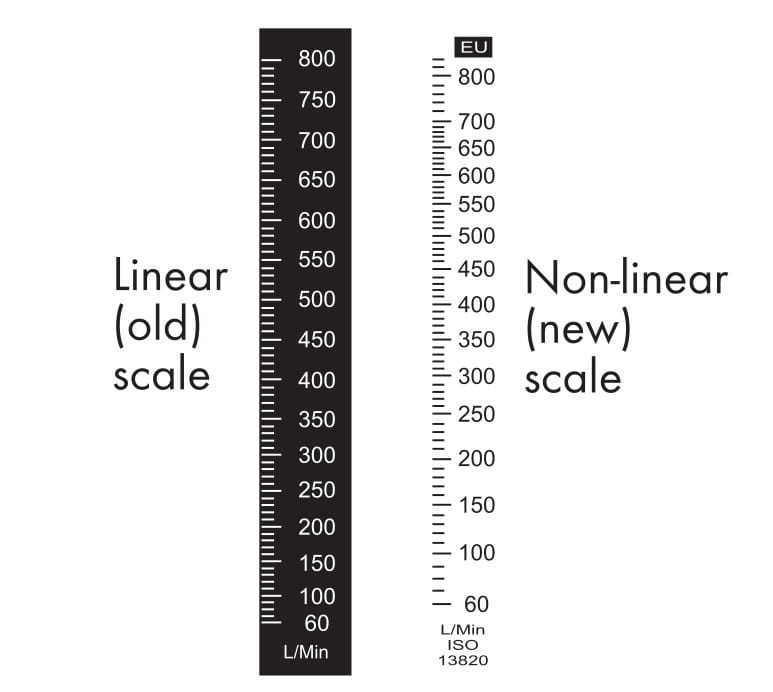
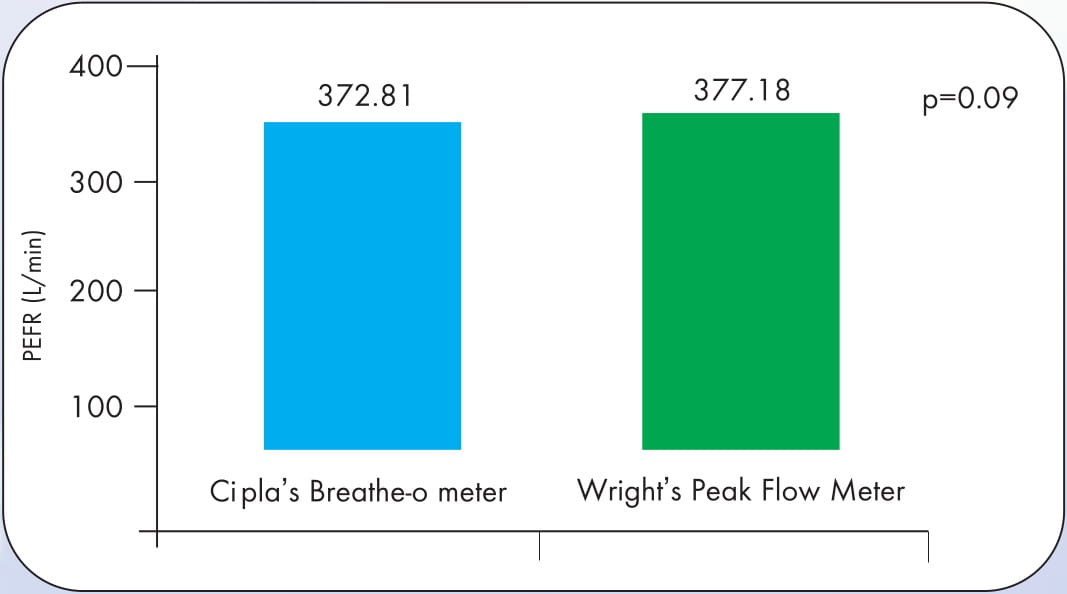
A study conducted by the Chest Research Foundation at Pune# and presented at the European Respiratory Society's 2006 Annual Congress, validated the breathe-o meter by comparing the PEFR values between Cipla's breathe-o meter and Wright's Peak Flow Meter (EU scales)**. Cipla's breathe-o meter produced PEFR values that were reproducible and equivalent to those produced by the Wright's Peak Flow Meter.
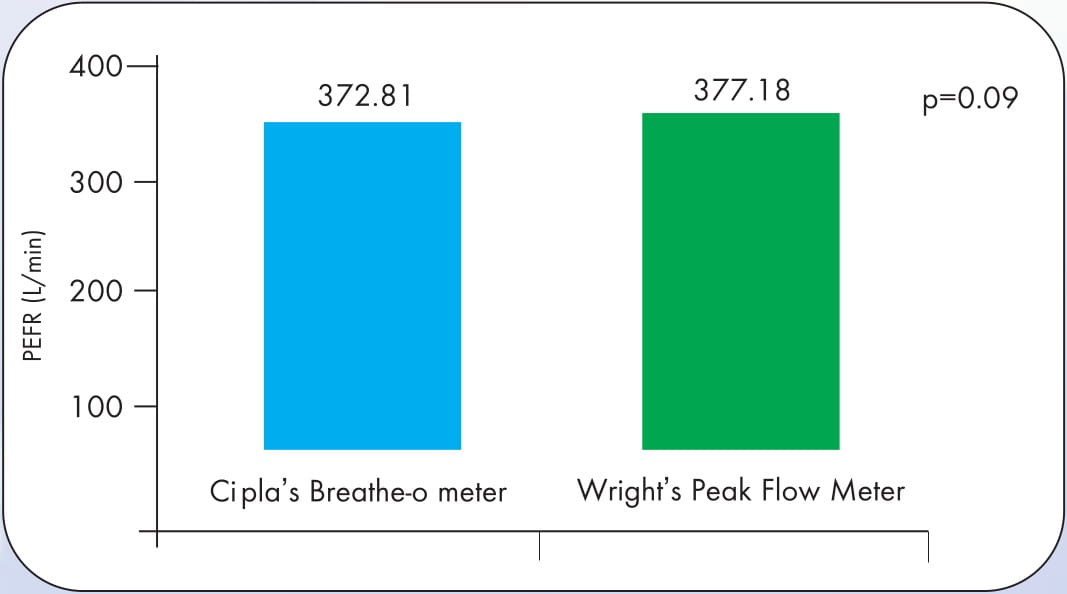
In this randomized, cross-over study, 24 subjects, healthy as well as asthmatic patients, were asked to perform three PEFR manoeuvres with two randomly picked breathe-o meters and two randomly picked Wright's Peak Flow Meters, all conforming to the EU scale. The mean differences in the PEFR readings with the Cipla's breathe-o meter and Wright's Peak Flow Meter were not significant. The values were also not different, whether patients or healthy subjects were tested. Also, there was no difference in the mean PEFR values obtained between the breathe-o meter and Wright's Peak Flow Meter (4.37 ± 12.4 L/min;p>0.05). There were no differences in the mean PEFR values, in the range of 300 to 500 L/min and >500 L/min, between the two devices.
The Cipla's breathe-o meter was found to be robust and showed PEFR values that were comparable to the Wright's Peak Flow Meter.
STEP 1: See whether the mouthpiece is fitted into the breathe-o meter. If not, attach it.

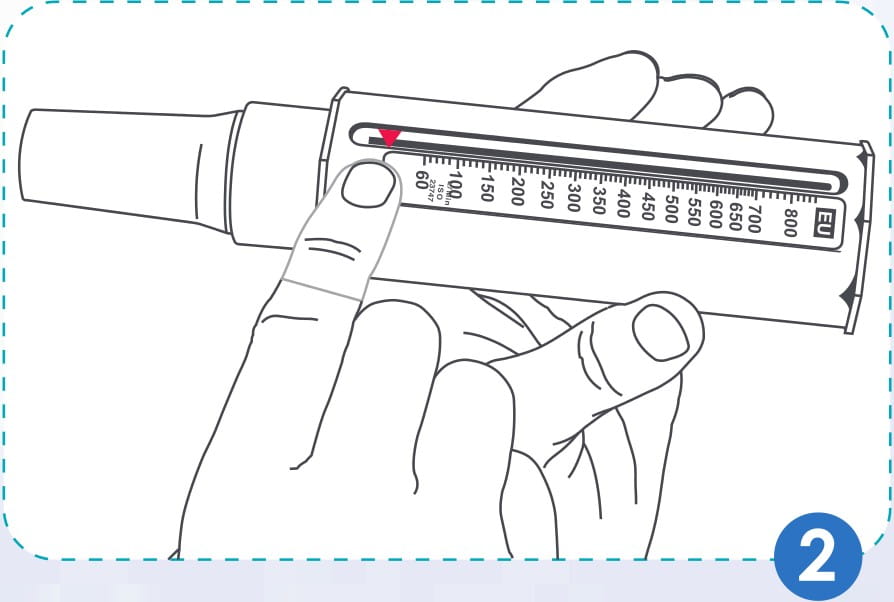
STEP 2: Move the pointer along the slot towards the mouthpiece till it does not move any further.
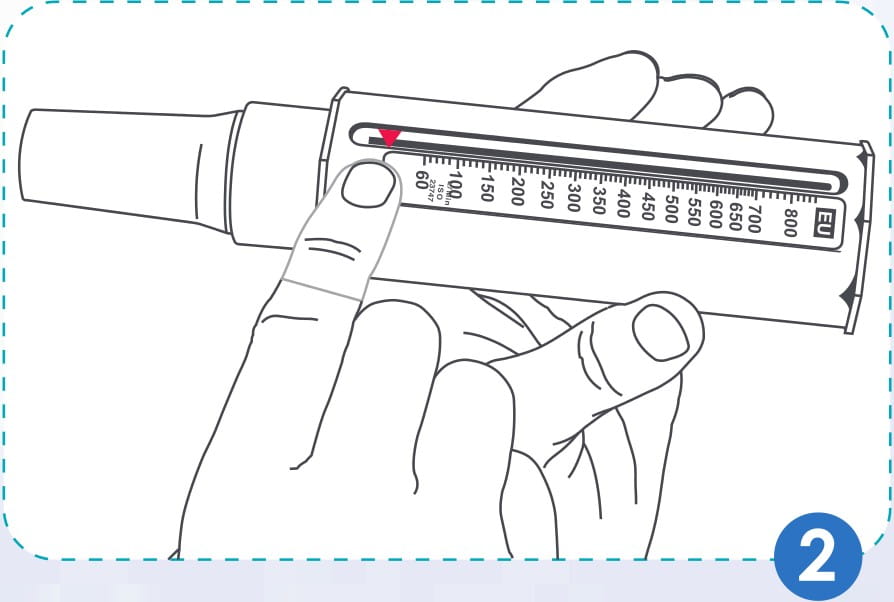
STEP 3: Hold the breathe-o meter so that the fingers are away from the scale & slot. Do not cover the holes at the end of the breathe-o meter. While holding the device do not press hard with the fingers because this may damage the device and affect the reading.

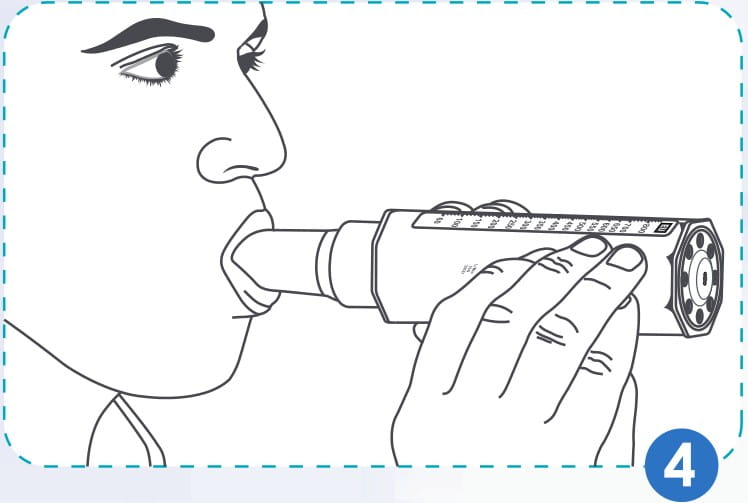
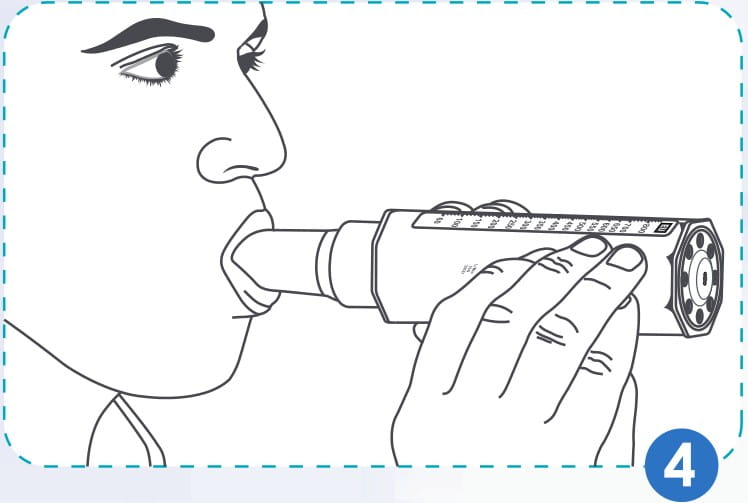
STEP 4: It is better to take the PEFR reading while standing up. Then, place the mouthpiece of the breathe-o meter in the mouth between the teeth. Keep lips closed firmly around the mouthpiece. Blow out just once, as hard and fast as you can. Do not put tongue inside the mouthpiece while blowing into the breathe-o meter. Please note that coughing or spitting into the breathe-o meter may affect the readings and should be avoided.
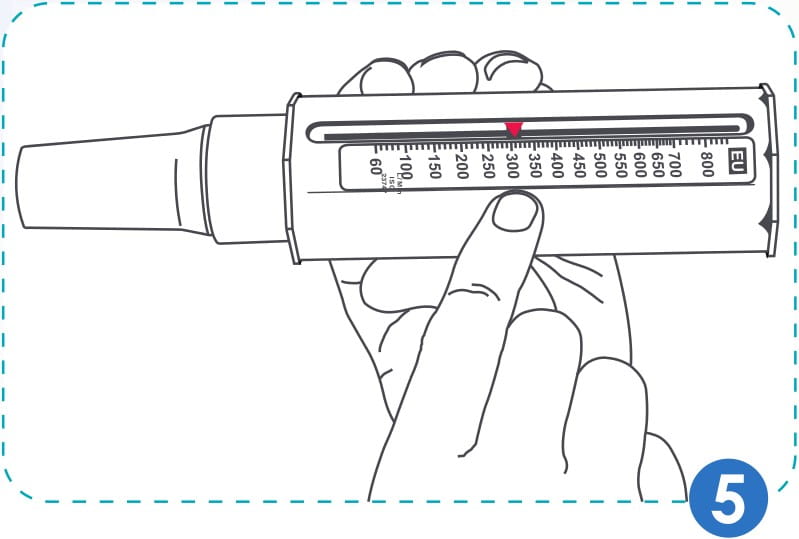
STEP 5: Note where the pointer has stopped on the scale. That number is the PEFR reading.
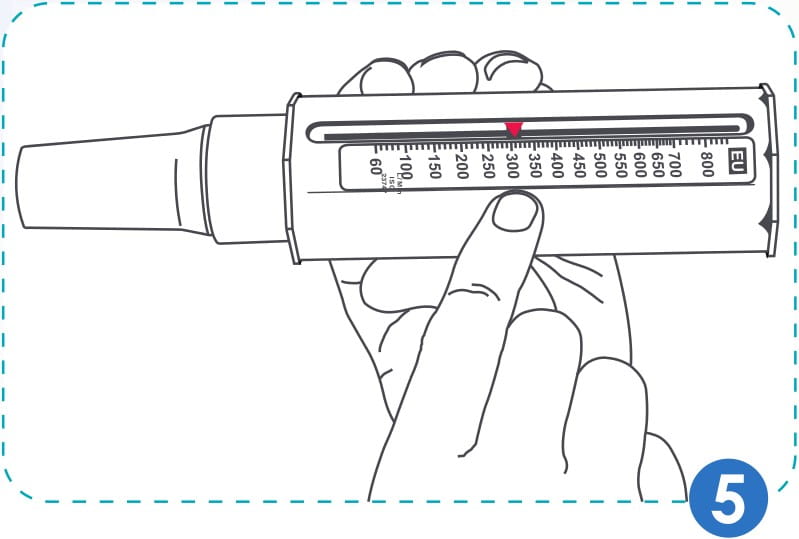
STEP 6: Repeat Step 2 to 5 two times more, so as to obtain three readings. The highest of the three readings is the PEFR reading. You should take the readings at least twice a day, first thing in the morning and then at bedtime, or as directed by your doctor.
PEFR readings should be repeated thrice in the manner described above. The best (i.e. highest) of the three readings is noted as the PEFR value for that test. At home, ideally, the PEFR should be measured twice a day, i.e., best of three efforts in the morning and best of three efforts at bedtime, before taking the prescribed medication.
It is important to keep a record of the PEFR values. This can be done by plotting the morning and evening values on a chart. By joining the dots over a period of time, the day-to-day variations in the PEFR can be seen.
PEFR monitoring can be effectively used to objectively understand the response to therapy instead of relying only on symptoms.
The PEFR measured before and after treatment may show how effective the medicines are and help to adjust the dose. Also, the patient gets an objective record of his/her lung function and this helps in improving the patient's compliance to the prescribed therapy.
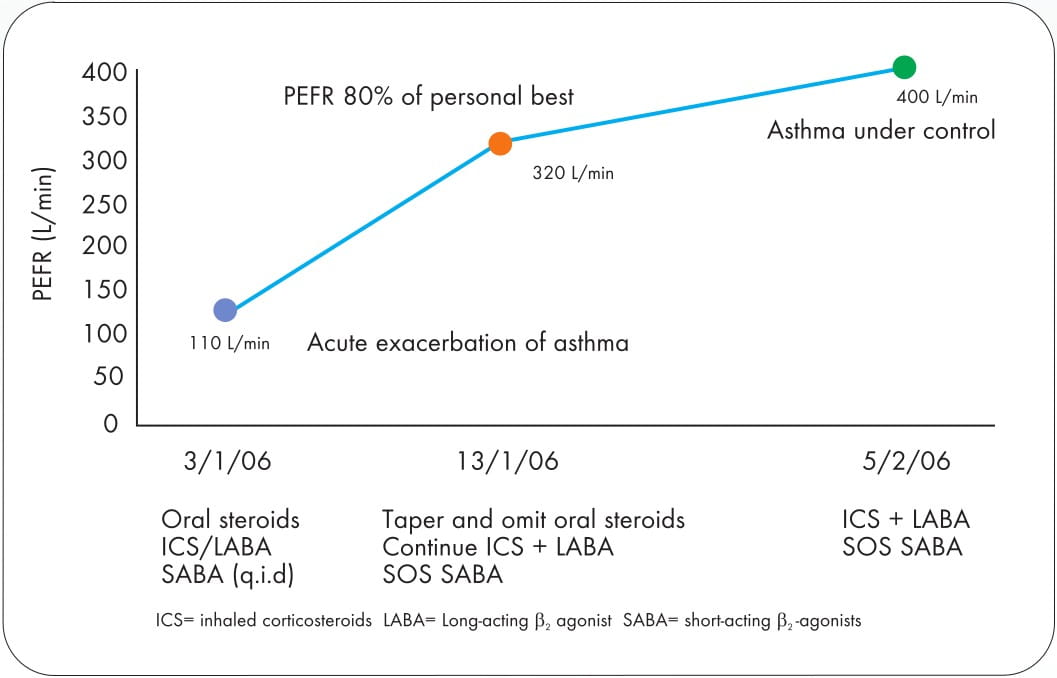
The following is a case study of a patient presenting with an acute exacerbation and started off on oral steroids.
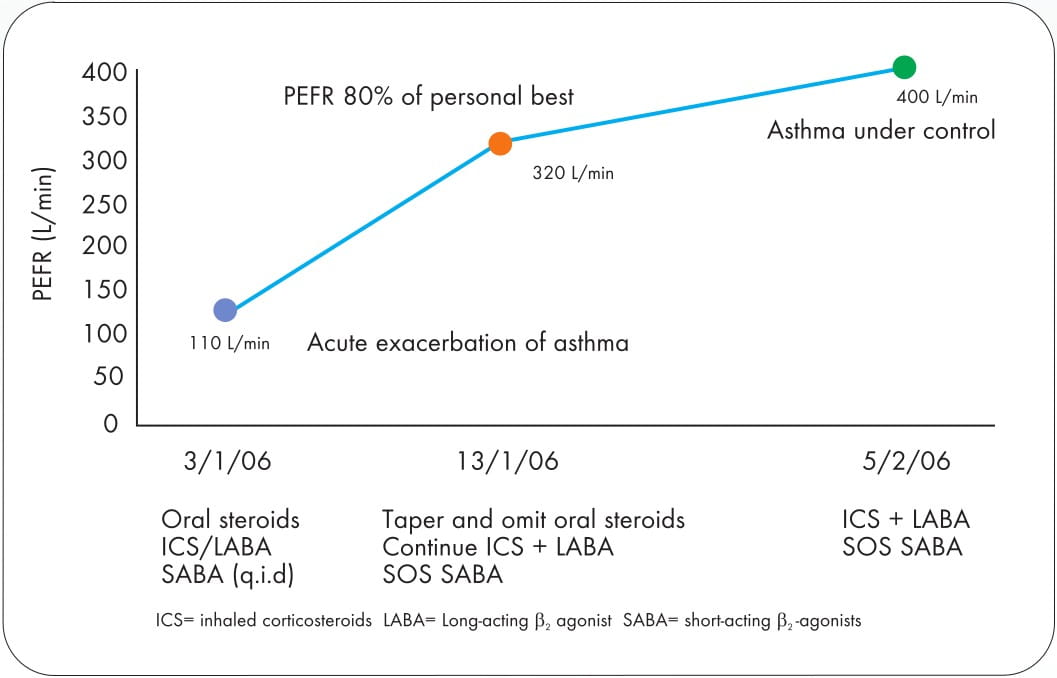
On follow-up, the patient showed an improvement in condition, judged on the basis of the PEFR, and the treatment was adjusted accordingly.
The personal best PEFR value is very useful for monitoring the disease regularly. Each time the patient visits the clinic, his/her PEFR is noted and compared with the "personal best". Values persistently below 20-30% of the personal best would indicate worsening control of asthma.
PEFR readings taken regularly at home can give a warning of an impending attack of acute exacerbation even before it starts manifesting symptomaticaly. At this stage, increasing the dose of inhaled steroids (4 times) along with bronchodilators may reduce the risk of an exacerbation.
A confirmation of occupational asthma may be successfully achieved by lung function measurements, such as serial measurements of the PEFR at work and away from work (single measurements are less sensitive than serial measurements). A similar approach can be used to evaluate the influence of potential allergens within the home, e.g., pollen, fur, dust, cats, viral infections, etc.
Reversibility
- Measure the PEFR reading (best of three blows).
- Administer a bronchodilator like salbutamol (asthalin)/levosalbutamol (levolin) or, two puffs with a metered dose inhaler (MDI) or one inhalation of a rotacap with a Rotahaler / Revolizer.
- Wait for 15-20minutes.
- Measure the PEFR of the patient again. If there is a ≥20% increase in the PEFR when measured after administering a bronchodilator, it indicates a significant degree of reversible airway obstruction, and a possible diagnosis of asthma.
The PEFR varies naturally at different times of the day. The lowest PEFR is usually recorded in the early morning and the highest in the evening. The difference between the highest and the lowest PEFR, expressed as a percent of the highest PEFR, is termed as diurnal variability.
Diurnal variation in the PEFR of more than 20%, averaged over a period of at least 14 days, suggests a diagnosis of asthma.
In many chronic ailments, it has been shown that using objective methods of monitoring the disease improves adherence to therapy since patients can actually see the difference the treatment is making. The breathe-o meter is a simple instrument with which patients can observe how well their lungs are functioning and this can help doctors to better explain the importance of taking treatment regularly even in the absence of symptoms.
The breathe-o meter has a special role in paediatric practice. It is often found that children either under-perceive or over-perceive their symptoms. The problem is further compounded by apprehension on part of the parents. Hence, correctly understanding the diagnosis, severity and response to therapy in asthmatic children is very difficult and often misguiding unless some objective tool for measuring the lung function is used. Children above the age of 4 to 5 years can safely and reliably use a breathe-o meter.
However, readings should preferably be taken under parental or doctor's supervision. These readings should be recorded and communicated to the child's doctor at each clinic visit.
Also, some children with asthma present only with exercise-induced symptoms. In this group, exercise testing in conjunction with the measurement of airflow limitations (PEFR) can be most helpful in establishing a firm diagnosis of asthma.
- Involve the patient in the decision making.
- Provide simple instructions about using the breathe-o meter, recording the PEFR and taking appropriate action.
- Use PEFR monitoring as a tool for the patients to take control of their asthma management.
- Show poor perceivers the relevance of PEFR monitoring.
It is not necessary to clean the breathe-o meter after each use. Cleaning once a month should be enough. Cleaning is simple and is important to maintain the accuracy of the breathe-o meter.
- Remove the mouthpiece and soak both the parts (mouthpiece and the breathe-o meter) in a warm water mixed with liquid soap solution for 2-3 minutes, as shown in the figure. Do not boil/autoclave the device.

- Shake both parts inside the solution to ensure thorough cleaning. Do not use a bottle brush or any other object to clean the parts.
- Rinse again in clean water and shake the breathe-o meter gently to remove excess water.
- Leave both parts to air-dry. Do not insert cloth or paper towels into the meter to speed up the drying process. Do not expose to heat.
When not in use, protect the breathe-o meter from dust, dirt and moisture by always placing it back inside the box provided.
- You can examine the breathe-o meter periodically to see if it is functioning properly.
- The breathe-o meter should be checked to see if there are any foreign particles inside; if so, the cleaning instructions should be followed.
- The indicator should move smoothly and freely but remain in place when moved to a position on the scale
Do not drop the breathe-o meter, as it may affect the readings of the meter.
- The breathe-o meter should be replaced at the end of 1 -2 years, depending upon single use or multi-patient use.
A damaged meter should not be used and it should be replaced immediately.
Do not allow children to play with the breathe-o meter as it may alter its function and/or overall reliability.
- When the breathe-o meter is used repeatedly as a screening device, patients should be instructed to inhale before placing the meter in their mouth. Always use disposable mouthpieces for this application.
- Frequent washing of the breathe-o meter would be required.
1. Med J Aust 1996; 164:727-730
2. Airways J 2004; 2(2):80 -2
3. J Allergy Clin Immunol 1991; 87(1):120-128
4. Global Initiative for Asthma (GINA)-2011
5. BMJ 1991; 302:738
6. http://www.aaaai.org/patients/publicedmat/tips/whatispeakflowmeter.stm (Accessed on 20th February, 2011)
7. http://www.patient.co.uk/showdoc/23069154 (Accessed on 20th February, 2011)
8. http://www.peakflow.com/portal_nav/nurse-docior/index.html (Accessed on 20th February, 2011)