Complementing COPD Management Through Smoking Cessation
Introduction
India has the second largest population (1,210 million) and tobacco users (275 million) after China. One out of two smokers who smoke throughout their lifetime will die from a disease related to smoking. Smoking is the leading cause of chronic obstructive pulmonary disease (C OPD). Tobacco smoking, therefore, represents a major global and nationwide public health issue.
Stopping smoking reduces the risk of developing COPD and is an essential treatment for this inflammatory disease. As smoking cessation slows the rate of decline in lung function, improves symptoms and potentially reduces the number of exacerbations in people with COPD, addressing this issue is of utmost importance in current smokers entering pulmonary rehabilitation. A strong dose-response relationship between the intensity of counselling therapy and its effectiveness has been recently observed in many studies.
When added to a 3-month rehabilitation programme, individual counselling and nicotine replacement therapy (NRT) has yielded a smoking cessation rate of 68% at 12 months.
This was considerably greater than that reported in a group that received individual counselling and NRT without rehabilitation (32%). Thus, the combination of high-intensity behavioral interventions and medication treatments (NRT, varenicline, bupropion) would be the most effective strategy for smokers with COPD entering a pulmonary rehabilitation programme. Two factors have been observed to predict the success of the attempt to quit in smokers with COPD: a strong motivation/counselling to quit and the use of smoking cessation medications.
Smoking Cessation and Counselling
Smoking cessation is the most effective strategy for prevention of COPD. Quitting smoking can prevent or delay the development of airflow limitation, or reduce its progression, and can have substantial effect on subsequent mortality. Among the COPD patients, 38-77% are smokers. Their daily cigarette consumption and level of nicotine dependence are often high. Counselling alone or counselling along with medication is used for smoking cessation. Significantly high continuous abstinence rates are seen with the medications as compared to counselling alone.
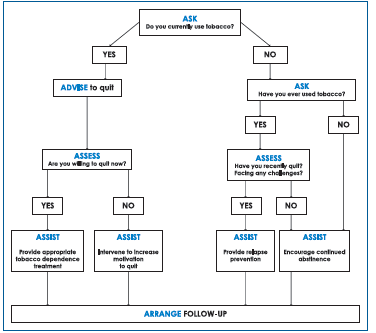
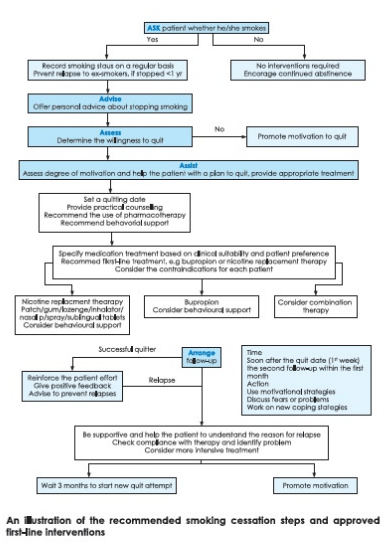
Counselling delivered by physicians and other professionals significantly increases quit rates over self-initiated strategies. Even a brief (3-minute) period of counselling to urge smoker to quit results in smoking cessation rates of 5-10%. The National Cancer Institute, USA, has formulated brief strategies to help the patients willing to quit and this includes a '5A' (ask, advise, assess, assist and arrange)-based intervention in a primary care setup. The GOLD guidelines 2016 have re-framed it as follows:
- ASK: Systematically identify all tobacco users at every visit. Implement an office-wide system that ensures that for every patient at every clinic visit, tobacco-use status is queried and documented.
- ADVISE: In a clear, strong and personalized manner, urge every tobacco user to quit.
- ASSESS: Determine willingness to make a quit attempt. Ask every tobacco user if he or she is willing to make a quit attempt at this time, e.g. within the next 30 days.
- ASSIST: Aid the patient in quitting. Help the patient with a quit plan; provide practical counselling; provide intra-treatment social support; help the patient obtain extra-treatment social support; recommend the use of approved pharmacotherapy except in special circumstances; provide supplementary materials.
- ARRANGE: Schedule follow-up contact either in person or via the telephone.
Pharmacological Intervention
Pharmacological intervention is indicated when counselling is not sufficient to help patients quit smoking. Pharmacotherapies can be divided into replacement therapy, antagonist therapy, therapies to make drug intake aversive and non-nicotine medications that mimic nicotine effects. Various drugs used are shown in Table.
|
Pharmacotherapy |
Dosage and Duration |
|
Bupropion |
150 mg OD for 3 days followed by 150 mg BD for 7 to 12 weeks |
|
Nicotine patch |
21 mg/ 24 hours for 4 weeks, then 14 mg / 24 hours for 2 weeks, then 7 mg / 24 hours for 2 weeks |
|
Nicotine gum |
For 1-24 cigarettes-2 mg gum (upto 24 pieces/day) for 12 weeks For > 25 cigarettes-4 mg gum (Upto 24 pieces/day) for 12 weeks |
|
Nicotine inhaler |
6-16 cartridges/day for 6 months |
|
Nicotine nasal spary |
1-2 doses/hour for 3 to 6 months |
|
Clonidine |
0.15 mg/day to 0.75 mg/day for 12 weeks |
|
Nortryptyline |
75 mg to l 00 mg/ day for 12 weeks |
Nicotine Replacement Therapies (NRT)
NRT consists of appropriate first-line agents. Numerous studies indicate that NRT in any form (nicotine gum, inhaler, nasal spray, transdermal patch, sublingual tablet, or lozenge) reliably increases long-term smoking abstinence rates. NRT is more effective when combined with counselling and behavior therapy.
Nicotine gum contains nicotine, which is slowly released inside the mouth and gets absorbed into the circulation from there. Through circulation, the nicotine reaches the brain - but not as quickly as it reaches the brain when taken through cigarette smoke.
The recommended dosage of nicotine gum is outlined as follows -
- For those smoking 1-24 cigarettes per day, 2 mg gum and for those smoking >25 cigarettes per day a 4 mg gum is recommended.
- One gum piece is to be chewed for 30 minutes every 1 or 2 hours and not more than 25 gum pieces per day are to be chewed.
- Duration of treatment is 12 weeks.
Side effects are soreness and dyspepsia.
A nicotine inhaler doubles the smoking cessation rate as compared to a placebo inhaler. Duration of therapy is 6 months with dose tapering in the last 3 months. Local irritation, cough and rhinitis are frequent side effects.
Nicotine nasal spray more than doubles the smoking cessation rate as compared to placebo nasal sprays. The dose is one spray of 0.5 mg into each nostril starting with one to two doses per hour to about five doses per hour according to symptom re lie f. Duration of therapy is 3-6 months. Side effects are nasal irritation, nasal congestion and a dependence potential in 15-20% of the patients in terms of length of use more than the recommended duration of 3-6 months.
A nicotine patch doubles the smoking cessation rate as compared to a placebo patch. The dose is a 16- or 24-hour patch that is to be applied for 8 weeks. Side effects are skin reactions and insomnia. The patch sites need to be rotated and 1% hydrocortisone has to be applied to counter skin reaction. Use of a 16-hour patch is recommended for those who suffer from insomnia. The patch is generally favoured over the nicotine gum because it requires less training for effective use and is associated with fewer compliance problems.
Medical contraindications to NRT include unstable coronary artery disease, untreated peptic ulcer disease, and recent myocardial infarction or stroke .
Medications that Mimic Nicotine Effects
- Bupropion SR: Bupropion SR is a non-nicotine medication with an abstinence rate twice that of the placebo. It acts by blocking the neural uptake of dopamine and noradrenaline. The drug is generally well tolerated in cardiovascular disease patients. Insomnia (35-40%) and dry mouth (10%) are the most common adverse events. It is contraindicated in seizure disorders, eating disorders and if a patient has used a MAO inhibitor in the past 14 days. It is given at a dose of 150 mg OD for 3 days; then 150 mg BD is continued for the next 7-12 weeks following the quit date, which is preferably between the first or second week of treatment. Consider giving maintenance therapy for 6-12 months in selected patients. It has been found to be associated with minimal post-cessation weight gain and is to be preferred in patients with depressive ideation. It has proven to be superior to NRT.
- Varenicline: Varenicline is a new nicotinic acetylcholine-receptor partial agonist that aids smoking cessation by relieving nicotine withdrawal symptoms and reducing the rewarding properties of nicotine, and it has been demonstrated to be safe and efficacious. The dose is 0.5 mg once a day for 1-3 days, then 0.5 mg twice a day for 4-7 days, followed by 1 mg twice a day from day 8 to the end of treatment, which is for a duration of 12 weeks
- Clonidine: Clonidine is a post-synaptic-2-agonist that dampens sympathetic activity originating at the locus ceruleus. Clonidine at doses of 0.1-0.4 mg/day for 2-6 weeks has been found to be useful. The most common side effects of are dry mouth, sedation and constipation. Clonidine appears to increase the quit rates similar to NRT.
- Anxiolytics: Anxiety is a prominent symptom of nicotine withdrawal. Smoking decreases some measure of anxiety and may reduce stress-induced anxiety. So, temporarily replacing the anxiolytic effects of nicotine with another medication during the first week of cessation might make the cessation easier. Diazepam and beta-blockers have been widely used with mixed results. Buspirone is a serotoninergic agonist, which acts as an anxiolytic but produces mixed results, when used for smoking cessation. The advantage over the benzodiazepines is that it is non-sedating and does not have an addictive potential. It is given at a dose of 15-30 mg/day in divided doses.
- Antidepressants: Many antidepressants have been tried with varied results. These are helpful only when the patients have underlying depression.
- Stimulants: The aim is to replace the stimulant effects of nicotine (e .g. improved energy and concentration) with medication in the first week of cessation. The drugs that have been used are amphetamine and methylphenidate.
- Anorectics: Anorectics were used initially to combat post-cessation hunger and weight gain because these are the two most widely cited reasons for difficulty in stopping smoking. Encouraging results have been obtained with fenfluramine and phenylpropanolamine in short-term trials.
- Sensory replacement: Black pepper extracts, capsaicin, denicotinized tobacco, flavourings - all these decrease cigarette craving and withdrawals. A citric acid inhaler has also been developed and showed some promise in two clinical trials.
- Acupuncture: Acupuncture technique is also used in smoking cessation. One common rationale for using acupuncture for smoking cessation is that acupuncture can release endorphins that assist in cessation.
Antagonists
The goal of the antagonists is to prevent cigarettes from producing positive reinforcing and subjective effects.
- Mecamylamine: Mecamylamine is a non-competitive blocker of both central and peripheral nervous system nicotine receptors that decreases the positive subjective effects of cigarettes.
- Naltrexone: Naltrexone is a long-acting form of the opioid antagonist, naloxone. The rationale for using naltrexone for smoking cessation is that the performance-enhancing effect and other positive effects of nicotine may be opioid-mediated. A couple of studies have pointed out the beneficial effects of naltrexone. Still, a study with a large sample size is needed before it can actually be recommended for use in clinical practice.
Medications that make nicotine intake aversive
Medications in this class produce unpleasant events when the patient ingests them. Silver acetate combines with the sulphides in tobacco smoke to produce a bad taste. Silver acetate has been tested as a gum and as a pill. Compliance is very poor with this drug.
Key Points: Pharmacological Intervention
- NRT and bupropion SR are first-line treatments for smoking cessation. Smokers attempting to quit should be encouraged to use these therapies to aid cessation, except in the presence of contraindications
- Different types of NRT (nicotine gum, patch, inhaler, nasal spray, lozenge and sublingual tablets) are equally effective as smoking cessation treatments.
- Combining the nicotine patch with a self-administered form of NRT can be more effective than a single form of NRT.
- NRT should be used to aid cessation in all smokers with COPD, regardless of disease severity and the number of cigarettes smoked.
- Combined treatment with bupropion SR and NRT might be more effective in heavy smokers.
- Both NRT and bupropion SR are effective and well tolerated in smokers with stable cardiovascular disease and in COPD patients.
- Varenicline might have an additional therapeutic effect as a smoking cessation treatment and is considered a second-line agent.
- Regular follow-up visits are important and are linked with a longer-term successful outcome.
Considering the above guidance for smoking cessation counselling and pharmacological intervention, a comprehensive treatment algorithm for smoking cessation has been outlined below:
Summary
- Smoking cessation is the most important step in the treatment of COPD.
- NRT with nicotine gum, inhaler, nasal spray, transdermal patch, sublingual tablet or lozenges has been found to increase long-term smoking abstinence rates.
- Varenicline and bupropion SR are pharmacologic agents for the treatment of tobacco addiction. Smoking cessation counselling is also effective to treat tobacco addiction.
- It has been reported that even a 3-minute period of counselling given to a smoker enables smoking cessation rates of 5-10%.
- Patients with COPD who smoke and receive intensive counselling or a combination of intensive counselling and NRT or bupropion SR demonstrate significantly higher abstinence rates.
Quit It to Beat It
Most times, the doctor's advice and counselling lead many patients to quit or significantly reduce their smoking habit. Unassisted smoking cessation in India is very low unlike in the West. In India, smokers might quit only after they get some diseases. Therefore, it is all the more important that doctors and other health professionals address tobacco as a serious risk to public health. Smoking cessation in the general population is usually preceded by smoking cessation among health professionals.
Further Reading
- Intern Med J 2006; 36:92-9.
- BMC Public Health 2013;13:47-52
- Rev Mal Respir. 2014;31 (10) :937-60
- J Assoc Physicians India. 2012; 60:53-56
- Indian J Med Res 2013;137:251-69
- Indian J Med Res 139, 2014, pp 484-486