Misoprostol for Prevention and Treatment of Postpartum Haemorrhage in Caesarean Deliveries
Expanding Horizons
Postpartum haemorrhage (PPH) is a major cause of maternal mortality in the developing world, accounting for one-third of maternal deaths. The leading cause is uterine atony, most often preventable by conventional uterotonics. However, the use of injectable uterotonics is not yet feasible in much of the developing world where deliveries still take place in rural areas with untrained birth attendants, along with other problems like instability at high temperatures, requirement of cold-chain storage and skills that some birth attendants might not possess.
Misoprostol, a prostaglandin E1 analogue, had primarily got approved for the prevention of non-steroidal anti-inflammatory drug (NSAID)-induced gastric ulcers. But now, the use of misoprostol in pregnancy has been nothing short of a revolution in reproductive health.
The use of misoprostol in the abortion and induction of labour has been widely established. The confirmed uterotonic action of misoprostol in early and late pregnancy led to its use in the third stage of labour. For prevention of PPH, misoprostol has been suggested as an alternative uterotonic since it is effective, inexpensive, can be taken orally, does not need refrigeration, can be easily administered, and has a long shelf-life.
Previous published studies have concentrated on the use of misoprostol in PPH after vaginal births. This booklet gives a new dimension to the use of misoprostol in the prevention and treatment of PPH after caesarean section. Though, these findings merit further investigations.
To observe the effects of misoprostol on reduction of postpartum bleeding in caesarean section.
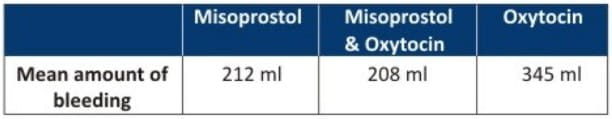
182 caesarean sections were randomised into three groups-
- Misoprostol group (n = 60) - 600 mcg misoprostol was given orally when peritoneum was incised.
- Misoprostol and oxytocin group (n = 64) - 600 mcg misoprostol was given orally and 20 IU oxytocin was injected into uterine muscle immediately after delivery of baby.
- Oxytocin group (n = 58) - 20 IU oxytocin was injected into uterine muscle and 20 IU injection IV immediately after delivery of baby.
The amount of bleeding within 2 hours after delivery was measured.
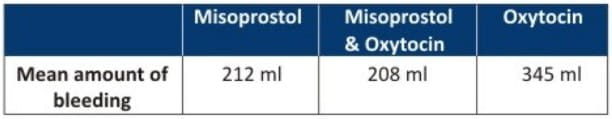
The difference was significant (P < 0.01) between misoprostol and oxytocin group, there was no difference between misoprostol and misoprostol plus oxytocin group.
Misoprostol is more effective than oxytocin in reducing postpartum bleeding.
Zhonghua Fu Chan Ke Za Zhi. 1998;33(7):403-5.
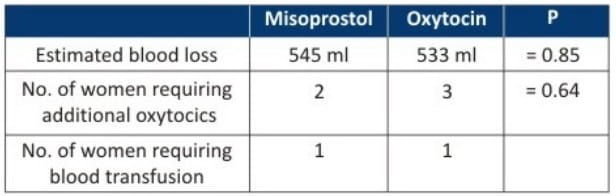
To investigate whether 500 mcg oral misoprostol given immediately after delivery of the neonate at caesarean section is as effective as a bolus IV injection of 10 IU oxytocin in stimulating uterine contractions and thereby reducing blood loss.
40 women undergoing elective or emergency caesarean section were included in a placebo-controlled randomised trial.
- Group I received oral misoprostol 500 mcg and a placebo IV bolus
- Group II received IV oxytocin 10 IU and oral placebo tablets.
Main outcome measures - estimated blood loss at caesarean section, drop in serum haemoglobin, need for additional uterotonic agents.
No significant difference was found between the two groups in -
- Estimated blood loss (p = 0.75)
- Decrease in haemoglobin (p > 0.05)
- Requirement for additional oxytocics (p > 0.05)
- Need for blood transfusion (p > 0.05)
- Degree of shivering (p> 0.05)
Oral misoprostol could be used as an alternative oxytocic agent for the third stage at caesarean section.
Aust N Z J Obstet Gynaecol. 2001;41(4):411-4.
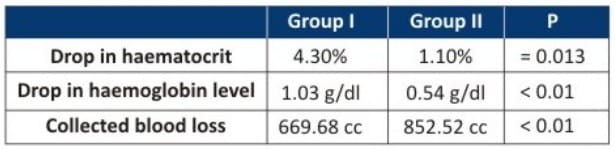
To assess the benefit of sublingual misoprostol in addition to standard oxytocin in the prevention of PPH at caesarean section.
This was a prospective randomised controlled clinical trial conducted from March to June 2007 at the department of obstetrics-Sousse Tunisia, including 250 single low risk pregnant women undergoing caesarean section at gestational age >32 weeks gestation.
At cord clamping, patients were randomly assigned to receive either-
- Group I - Sublingual misoprostol 200 mcg with 20 IU oxytocin IV (bolus 10 IU and infusion 10 IU in 500 ml Ringer Lactate), or
- Group II - Only oxytocin at the same dose.
Main outcome - total blood loss assessed by decrease in perioperative haematocrit.
Secondary outcomes - measure of collected blood loss, drop in haemoglobin level, additional oxytocin, side-effects and postoperative complications.
The two groups were similar in demographic and obstetrical patient characteristics.
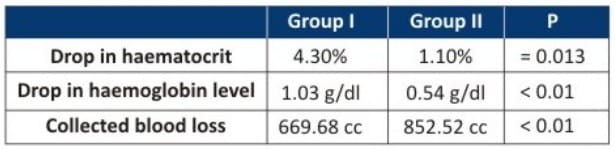
- Need for additional oxytocin and postoperative complications rate were more frequent in group II than in group I but the differences weren't significant.
- Rate of transient shivering, nausea and fever was significantly higher among women receiving misoprostol.
Sublingual misoprostol (in addition to oxytocin) is effective in prevention of PPH at caesarean sections when compared to oxytocin alone, without major side-effects.
J Gynecol Obstet Biol Reprod (Paris). 2009;38(7):588-93.
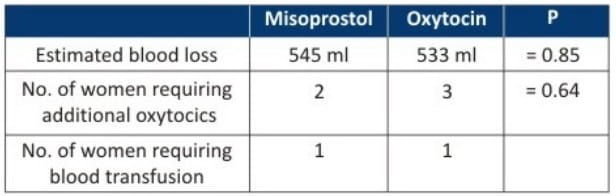
To randomly compare the effectiveness of oral misoprostol with IV oxytocin on blood loss during elective caesarean sections under regional anaesthesia.
During caesarean section, 60 pregnant women were randomised to receive either-
- Misoprostol 400 mcg orally, or
- Oxytocin 10 IU IV.
The primary outcome measure was intra-operative blood loss as estimated by physicians, and by values of preoperative and postoperative haemoglobin concentration and haematocrit.
Baseline characteristics in terms of age, body weight, parity, gestational age and indications for caesarean section were similar in both groups.
- Differences in preoperative and postoperative haemoglobin and haematocrit values were similar in both groups.
- No serious side effects were noted in either group.
Oral misoprostol appears to be safe and as effective as IV oxytocin in reduction of intra-operative blood loss during elective caesarean section under regional anaesthesia.
Acta Obstet Gynecol Scand. 2001;80(3):245-50.
To compare the effectiveness of oral misoprostol and IV oxytocin in reducing blood loss in women undergoing indicated or elective caesarean delivery under spinal anesthesia.
In this prospective, double-blind pilot study, 56 parturients who received 5 IU of IV oxytocin after cord clamping were randomised to further receive either -
- Group I - 800 mcg of misoprostol orally plus an infusion of normal saline solution (1000 ml over 8 h) supplemented with placebo, or
- Group II - An oral placebo plus an infusion of normal saline solution (1000 ml over 8 h) supplemented with 20 IU of oxytocin.
After adjusting for the sonographically estimated amniotic fluid volume, there was no statistical difference in blood loss between the 2 groups (1083 ml in the oxytocin group vs. 970 ml in the misoprostol group; P=0.59).
Oxytocin followed by oral misoprostol is as effective as an oxytocin injection followed by an oxytocin infusion in reducing postoperative blood loss after caesarean delivery and the protocol may be a safe, valuable, and cost-effective alternative to oxytocin alone. Visual estimation of intraoperative blood loss undervalues the effective value of misoprostol use by 30%.
Int J Gynaecol Obstet. 2006;95(1):2-7.
To determine the efficacy of misoprostol in cases of abnormal and pathologic hypotonic haemorrhage in the early puerperium as a result of hypotonia of the uterus.
- Group I - 50 women with vaginal or abdominal labour developing hypotonic abnormal/pathologic bleeding after the placental delivery were given misoprostol (200-400 mcg per rectum and/or per oral every 15 minutes).
- Group II - Control group without postpartum bleeding.
- Misoprostol resulted in uterine contraction and discontinuing the abnormal bleedings in both vaginal and caesarean deliveries.
- Mean blood lost in the next two hours period after vaginal labour did not differ with the blood lost of the normal labours (66 ml vs. 75 ml).
- In the caesarean deliveries, the blood lost after application of the misoprostol also did not differ with the blood lost after normal caesarean section (78 ml vs. 80 ml).
Misoprostol decreases the hypotonic uterine bleeding in the placental and early puerperal period. The significance of the misoprostol in the group of therapeutic events is determined by its fast therapeutic effect, convenient application and good tolerance.
Akush Ginekol (Sofiia). 2006;45(3):16-9.
To assess the efficacy of buccal misoprostol to decrease uterine atony, haemorrhage, and the need for additional uterotonic agents during caesarean delivery.
- Patients who underwent caesarean delivery were assigned randomly to either 200 mcg misoprostol or placebo placed in the buccal space.
- A dilute IV oxytocin infusion was given to all patients at delivery of the placenta.
Primary outcome variable - need for additional uterotonic agents.
A total of 352 women received random assignments. Demographic and intrapartum characteristics were similar between the groups. More women in the placebo group required 1 additional uterotonic agent (43% vs 26%; P < .01). There was no difference between the groups in the incidence of PPH or a difference in preoperative and postoperative haemoglobin level.
Buccal misoprostol reduces the need for additional uterotonic agents during caesarean delivery.
Am J Obstet Gynecol. 2005:192(5):1404-6.
To compare the effectiveness of sublingual misoprostol administered immediately after delivery of the neonate at caesarean section, with IV oxytocin infusion in prevention of uterine atony and thereby reducing blood loss at caesarean section.
100 women with singleton term pregnancy undergoing elective or emergency lower segment caesarean section under spinal anaesthesia were randomly allocated, soon after delivery of the neonate, to receive either -
- Misoprostol 400 mcg sublingually, or
- IV infusion of 20 units of oxytocin.
Main outcome measures - blood loss at caesarean section, change in haemoglobin levels, need for additional oxytocics and drug related side effects.
- Number of women who had blood loss exceeding 500 ml and the change in haemoglobin was comparable between the two groups.
- Incidence of side effects such as pyrexia, shivering and metallic taste was significantly higher in misoprostol group compared to oxytocin group.
Sublingual misoprostol appears to be as effective as IV infusion of oxytocin in reducing blood loss at caesarean section. However, occurrence of transient side effects such as shivering and pyrexia were noted more frequently with the use of misoprostol.
lnt J Gynaecol Obstet. 2006;92(2):106-10.
To evaluate a PPH treatment guideline, using rectally administered misoprostol.
A descriptive study was carried out in a tertiary referral center from January 2002 to March 2003. During this period, 2670 patients delivered.
- 41 (1.5%) with severe PPH unresponsive to oxytocin received 1000 mcg of misoprostol rectally while awaiting sulprostone.
- 28 had delivered by the vaginal route and 13 by caesarean section.
- Haemorrhage was controlled among 63% (26/41) of the patients within 10 minutes of the administration of rectal misoprostol.
- 15 (37%) patients received both misoprostol and sulprostone and no major adverse effects were noted when combining these two prostaglandins.
- Overall, haemorrhage was controlled among 87% (36/41) of the patients when oxytocics were combined with misoprostol and sulprostone.
- 5 patients (12%) did not respond to the combination of uterotonics and required a conservative surgical treatment.
Rectal misoprostol may be an effective second line treatment for the management of PPH unresponsive to oxytocin. No major side effects were observed when combining misoprostol with sulprostone. These findings encourage further research on rectal misoprostol in the treatment of PPH.
Gynecol Obstet Fertil. 2004;32(9):703-7.
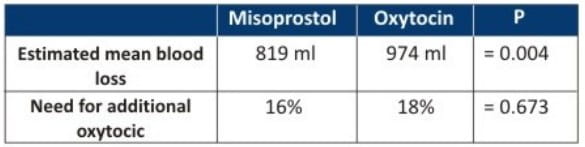
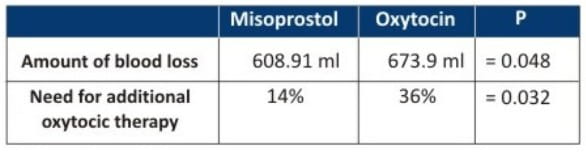
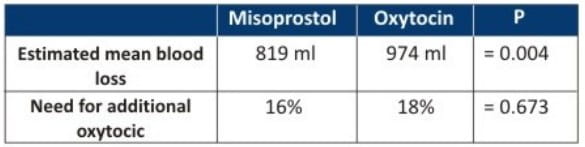
To study the effect of sublingual misoprostol vs. IV oxytocin in reducing bleeding after caesarean section.
- 100 singleton pregnant women underwent a caesarean delivery under general anaesthesia and were studied in terms of postpartum bleeding using oxytocin or misoprostol.
- Patients were randomly divided into two equal groups -
- Group I received two tablets of misoprostol 200 mcg sublingually
- Group II received IV infusion of 20 units of oxytocin at the rate of 10 cc/min immediately after delivery until full contraction of the uterine.
The amount of blood loss and the need to give additional oxytocin therapy was significantly lower in misoprostol group compared with oxytocin group.
- The efficacy of sublingual misoprostol is equivalent to that of low dose IV oxytocin in reducing PPH at caesarean section.
- Misoprostol has some other advantages like long shelf-life, stability at room temperature and oral use.
J Obstet Gynaecol. 2009 Oct;29(7):633-6.
To evaluate efficacy of misoprostol by vaginal route for the prevention of the obstetric haemorrhage and to know its side effects.
This was a randomised clinical trial conducted on 200 patients who had undergone caesarean. After the delivery -
- Group I was given placebo, and
- Group II was given 800 mcg misoprostol vaginally.
The requirement of additional uterotonics, drop in haemoglobin and haematocrit, and the side effects were compared.
- With misoprostol, the requirement of additional uterotonics was decreased to 50% and the drop in haemoglobin was seen in 39.6% of the patients.
- Drop in haemoglobin by 3g% was seen in 13% of the patients in placebo vs. 3% of the patients in misoprostol group. Drop in haematocrit was seen in 40.6% of the patients.
- In 7% of the patients in placebo and 1% of the patients in misoprostol group, the haematocrit fell by more than 10%. The side effects were few and not so serious.
The intrauterine combination of misoprostol and oxytocin reduces the post-caesarean blood loss and has few side effects.
Ginecol Obstet Mex. 2009;77(10):469-74.
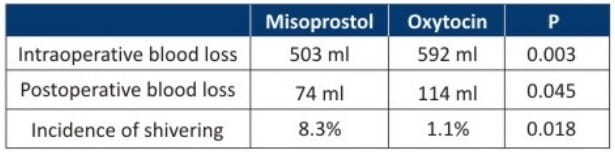
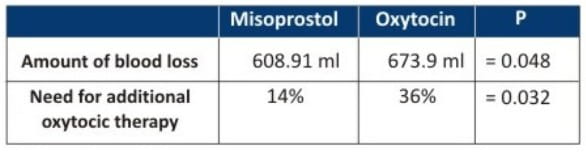
To compare the efficacy of rectally administered misoprostol with IV oxytocin infusion in preventing uterine atony and blood loss during caesarean delivery.
In this prospective, randomized, double-blind trial, 200 women undergoing caesarean delivery who did not have risk factors for PPH were randomly allocated to receive either -
- Group I - 800 mcg of misoprostol rectally and 8 ampoules of placebo injection at the time of peritoneal incision
- Group II - 4 placebo tablets and 8 ampoules of oxytocin injection each containing 5 IU of oxytocin.
Primary outcome measures - amount of intraoperative and postoperative (8 hours) blood loss and changes in haemoglobin levels 24 hours after delivery.
A total of 96 and 94 women were analyzed in the misoprostol and oxytocin groups, respectively. Intraoperative and postoperative blood loss was significantly lower in the misoprostol group than in the oxytocin group.
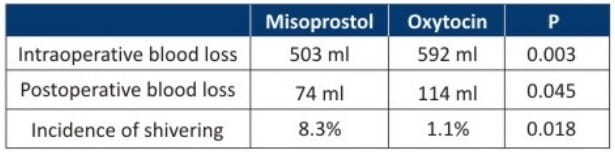
Rectal misoprostol appears to be an effective alternative to IV oxytocin in preventing blood loss for routine use during caesarean delivery.
Int J Gynaecol Obstet. 2010;109(1):25-9