Update on Osteoporosis
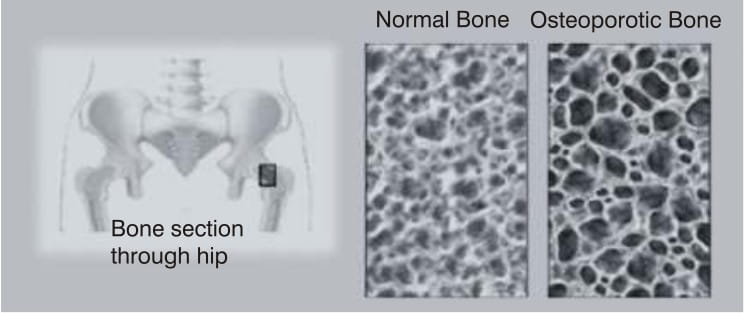
Osteoporosis is the most common bone disease in humans and is characterised by low bone mass, microarchitectural deterioration, compromised bone strength, and an increased risk of fracture. In osteoporosis, the absolute bone mass is so significantly reduced that fracture risk is increased even in the absence of significant trauma.
It is also a major cause of pain and disability worldwide. The number of people suffering from bone and joint diseases is expected to double within the next 20 years. It may even be greater due to longer survival and, consequently, larger number of older people in the population.
Osteoporosis is especially prevalent in older postmenopausal women. However, today, experts have finally come to the realization that osteoporosis can affect everybody, independent of sex and age.
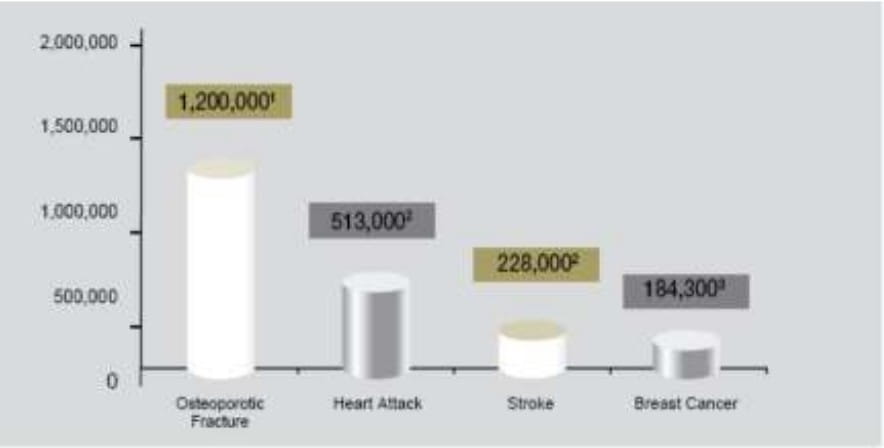
Enormous work and research on bone disorders done over the past 10-20 years has contributed greatly to our understanding of osteoporosis, its causes, prevention and treatment. Osteoporosis is now identified as one of the most important diseases affecting the human race, along with hypertension and diabetes. While every eighth woman suffers from breast cancer, every third woman sustains a fracture due to osteoporosis.
The aim of this article is to raise awareness and inform physicians across disciplines about this preventable and treatable disease.
Osteoporosis can occur in any racial group, although it is most common in Asians and Caucasians. In a study done at Chennai, it was noted that 58.6% of the postmenopausal women studied were osteoporotic. From the age of 50 years, a woman has the following risk for a fracture:
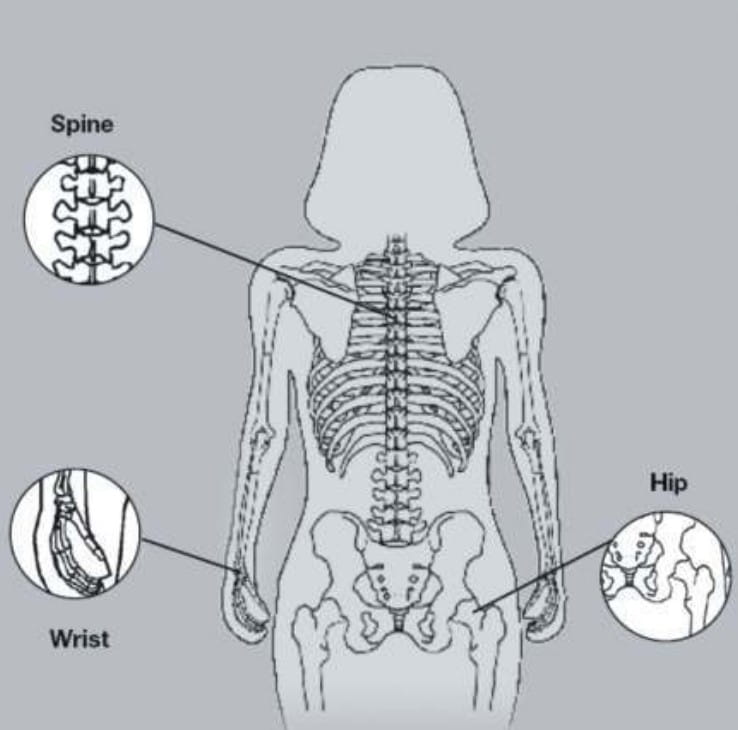
• Vertebral - 32% • Lower arm - 16% • Hip - 15%
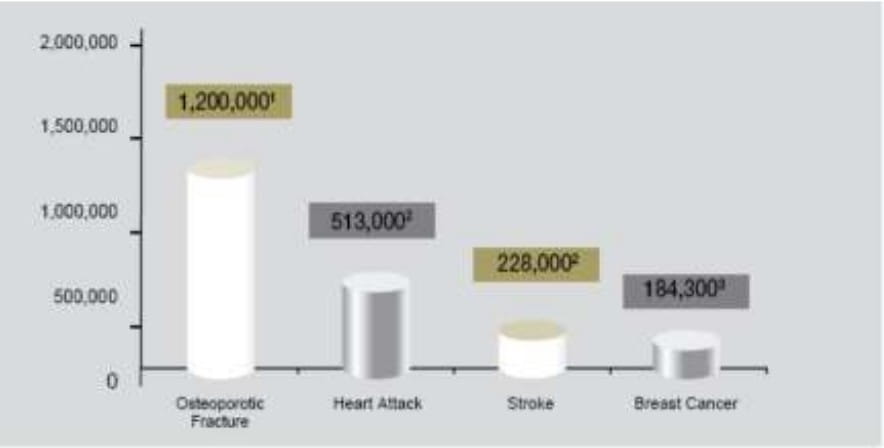
The burden of pain, physical disability, and reduced quality of life among osteoporotic women represents a major public health problem.
The cumulative lifetime risk of having an osteoporotic fracture is 13% among men and 40% among women. When all fractures are considered, the lifetime risk of experiencing >1 fracture is >50%. Many women who have one osteoporotic fracture will experience further fractures, partly because prior fracture is itself an important independent risk factor for future fractures. Furthermore, women with very low BMD have much higher risks than the average, and many of them will experience fractures if untreated.
Although all fractures are debilitating to some degree, hip fracture is the most serious consequence of osteoporosis.
A hip fracture poses an increased risk of mortality related to coexisting diseases such as stroke, heart failure, or chronic lung diseases, as well as to complications secondary to surgical treatment of the fracture. Nearly 50% of individuals with hip fractures never fully recover the mobility and independence they had previously, and an additional 25% require a long-term nursing facility or home care. Mortality after a hip fracture is estimated to range from 12% to 35%, more than that expected in the general population. The risk of a woman dying from a hip fracture (2.8%) is equal to that of dying from breast cancer and four times greater than that for endometrial cancer (0.7%). The highest mortality typically occurs within the first 6 months following a fracture; however, some studies show a sustained effect.
Vertebral fracture is the most common osteoporotic fracture and occurs earlier in life than hip fracture. Like hip fracture, vertebral fracture is associated with considerable morbidity. Approximately two-thirds of all vertebral fractures are not recognized clinically, but both diagnosed and undiagnosed vertebral fractures are associated with pain and impaired physical function. Declines in physical function and changes in appearance (kyphosis and height loss) contribute to social isolation and loss of self-esteem, impairing the quality of life.
Women who have had a spinal or non-spinal fracture are 2 to 6 times more likely to report difficulties performing activities of daily living than those without fractures. Furthermore, decreases in physical function often lead to an increased risk of falls and fractures and to the fear of falling, which further restrict activities and independence. Indeed, the economic costs of osteoporosis are as significant as those associated with other important diseases such as chronic obstructive pulmonary disease, myocardial infarction, stroke and breast cancer. These burdens will increase dramatically in the coming decades because of the growing population of elderly persons.
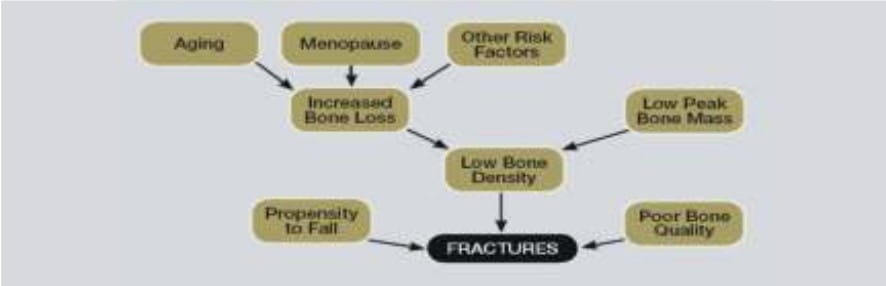
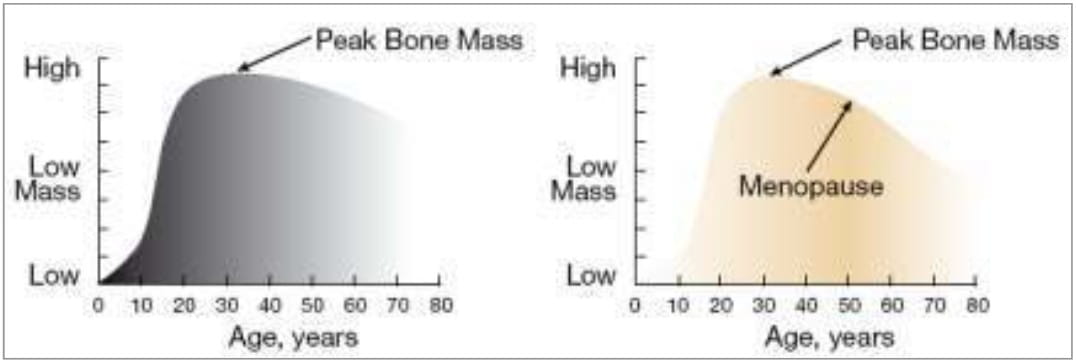
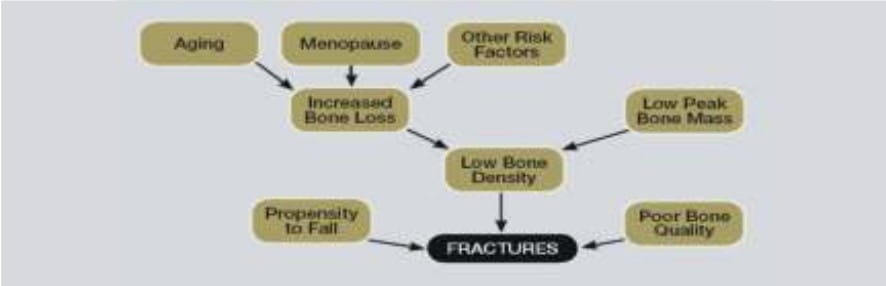
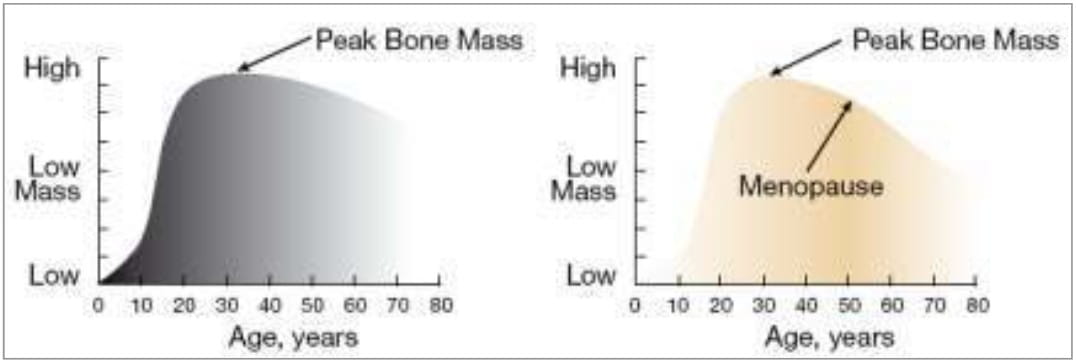
Bone tissue is in a constant state of remodelling where bone is being broken down by osteoclasts and rebuilt by osteoblasts. During childhood and young adult years, bone formation exceeds bone destruction; therefore, there is a steady increase in bone mass. However, between the ages of 25 and 35 years, humans reach an apex, which signifies their peak bone mineral density (BMD). This peak density is influenced by a number of factors including genetics, nutrition, exercise and hormones. After this age, the balance changes to favour osteoclastic activity.
Subsequently, both men and women lose BMD at a rate of approximately 3-4% per decade. This process continues throughout a man's life. However, among women, bone loss accelerates to approximately 9% per decade for 10 - 20 years following menopause, due to the decreased estrogen concentrations in the body, and then stabilises at a rate of 3-4% per decade.
Estrogen receptors are located throughout the body, including sites in bone tissue, the intestines, and the kidneys. Before menopause, estrogen interacts with these receptors and favourably affects bone remodelling and calcium balance. After menopause, serum estrogen levels drop, resulting in decreased estrogen receptor stimulation, increased production of cytokines, and increased osteoclastic activity. The remodelling balance is disrupted, and bone breakdown exceeds bone production, rendering the bone matrix unstable and increasing the risk of fracture.
Extracellular levels of calcium and phosphorus maintain the systemic regulation of bone remodelling. Parathyroid hormone and vitamin D are the key regulators.
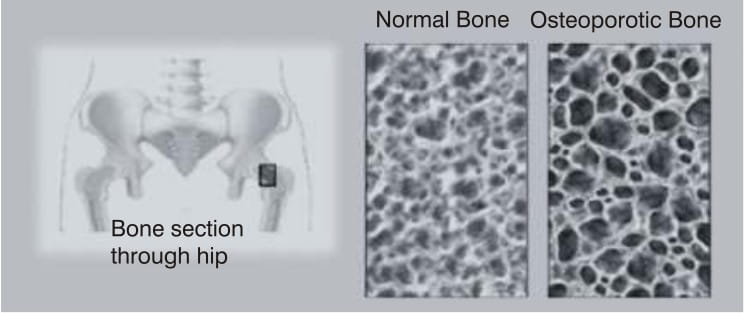
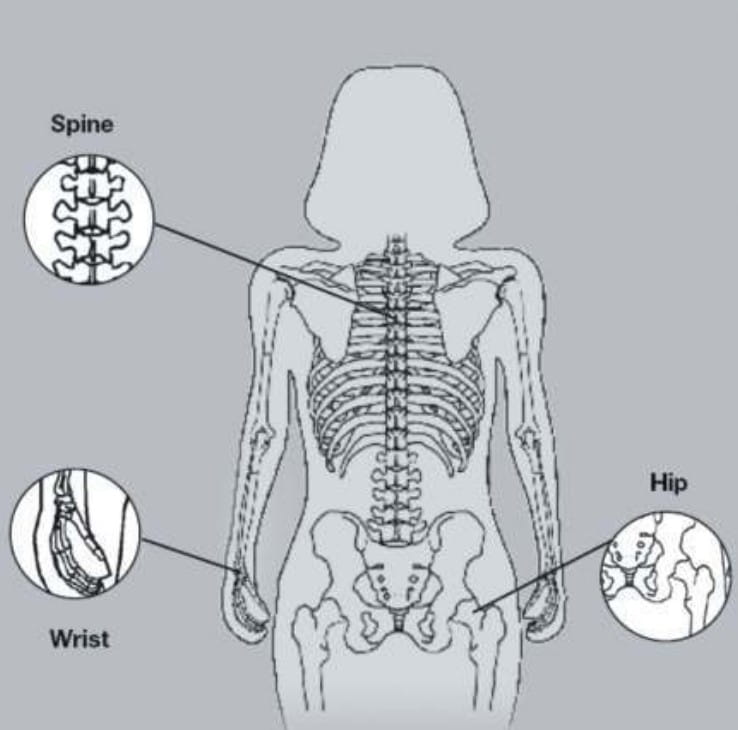
Common sites of fracture: There are two types of bones in the body, the cortical and the trabecular (or spongy) bone. Trabecular bone is more metabolically active. It is located in sites such as the vertebrae, at the end of long bones, in the wrist and ankle, and between the ribs. Therefore, these are the most common sites of osteoporotic fracture.
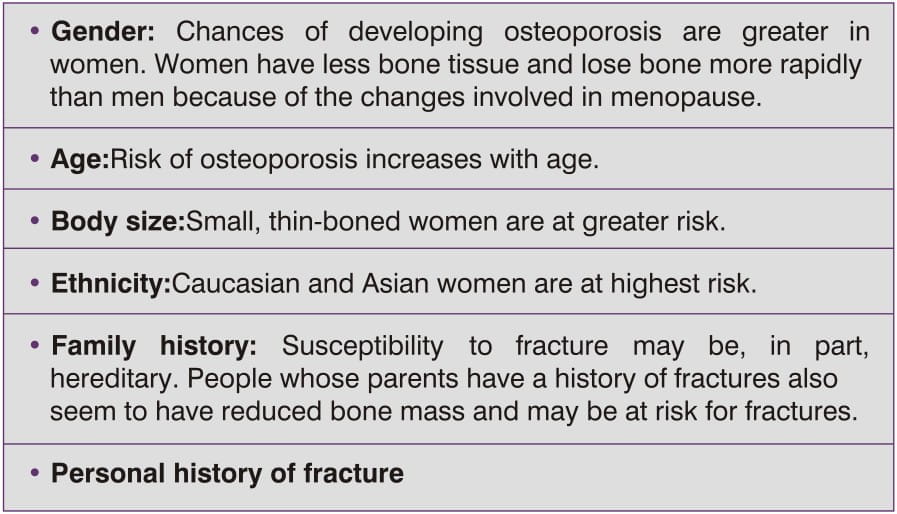
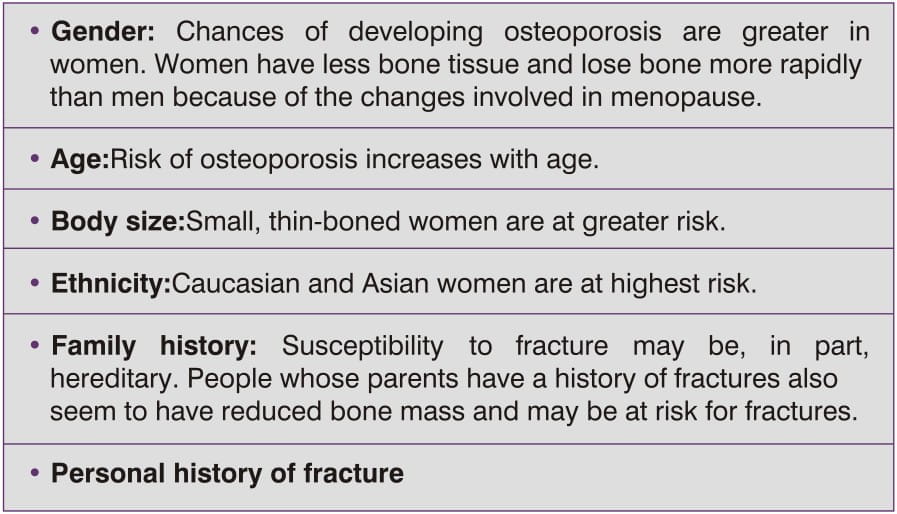
Osteoporosis is a preventable and treatable disease, but because there are no warning signs until a fracture occurs, many people are not diagnosed in time to receive effective therapy during the early phase of the disease. Certain factors are linked to the development of osteoporosis. Some of these are modifiable while others are not.
- Cigarette smoking
- Diet low in calcium/vitamin D
- Use of glucocorticoids, anticonvulsants and certain other drugs
- Excessive alcohol intake (>2 drinks per day)
- Sedentary lifestyle
- Estrogen deficiency at an early age (<45 yrs)
- Environmental risks (loose rugs, dark stairs, etc.)
- Poor eyesight
- Excessive sport
- Occupation - Astronauts
Osteoporosis can be clinically subdivided into
Deterioration of bone mass that is unassociated with other chronic illness.
Primary Osteoporosis can be further divided into
a) Postmenopausal (Type I) osteoporosis: This is the most common form of osteoporosis and it occurs in women 51-70 years of age as a consequence of cessation of ovarian function. The loss of bone actually starts years beforehand and increases at the time of menopause. Cessation of estrogen secretion leads to a decrease in IL-6 and other cytokines, which in turn leads to increased recruitment and activation of osteoclasts.
In addition, bone becomes more sensitive to the resorption stimulating action of parathyroid hormone. As a consequence, there is increased resorption of cancellous bone in the vertebra and hip bones, with a corresponding increase in risk of fractures.
This postmenopausal form of osteoporosis obviously occurs in women only, but men are also subject to increased bone resorption as a consequence of testosterone deficiency, though at a later stage in life.
b) Involutional (age-related, Type II) osteoporosis: Postmenopausal osteoporosis merges imperceptibly into the age-related type, which represents part of the aging process and includes increased osteoclastic activity. Study of bone biopsies taken from normal individuals of different age groups show that bone is not an atrophic tissue in the older age groups. It presents the picture of osseous remodelling. Causative factors for involutional osteoporosis are decreased mobility, defective vitamin D metabolism, insufficient calcium, and mild secondary hyperparathyroidism. This type of osteoporosis develops after 70 years of age and is now only twice as frequent in women as in men. Cortical bone, especially that of the femoral neck, radius and pelvic bones are involved. The arbitrary separation of osteoporosis into Type I and II, at this stage in patients' lives (>70 years), is of little practical value.
c) Idiopathic osteoporosis: This occurs in children and young adults, and the cause is not known.
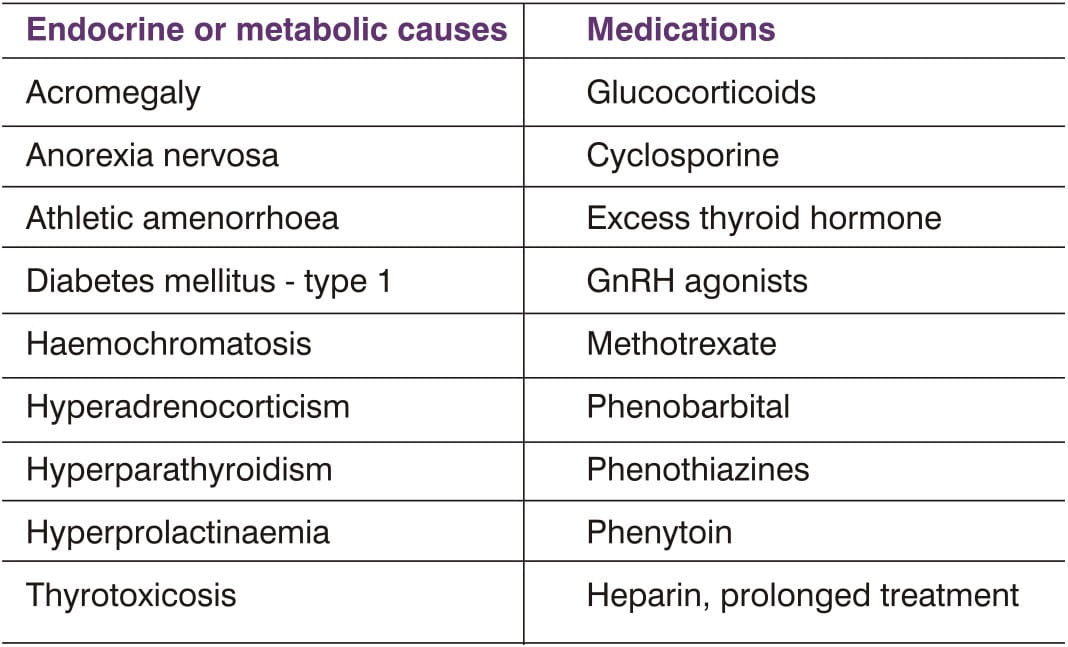
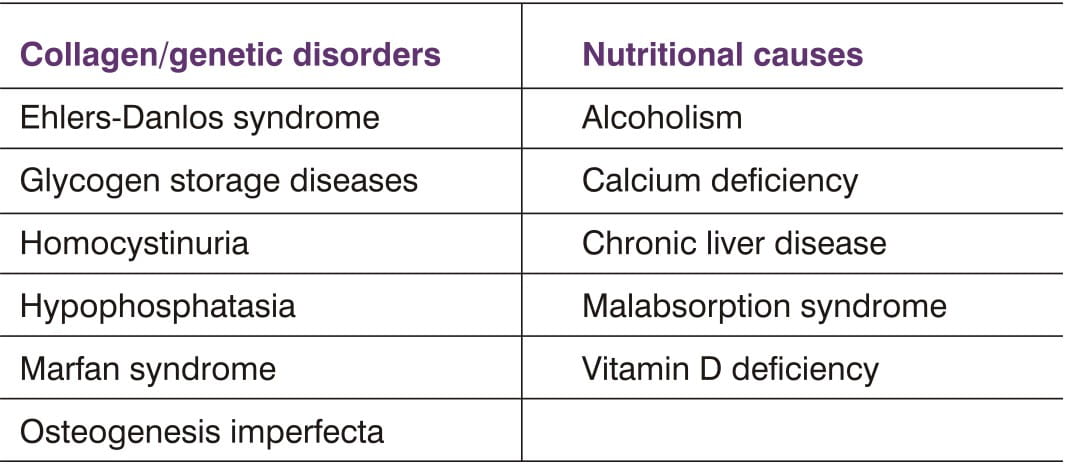
Secondary osteoporosis results from chronic conditions that contribute significantly to accelerated bone loss.
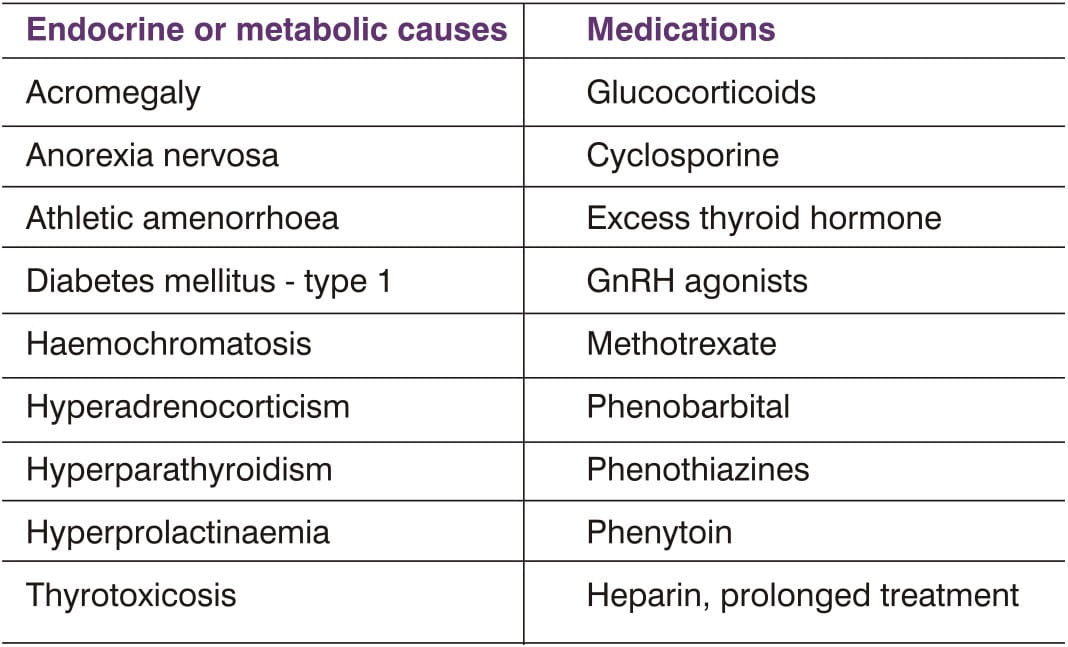
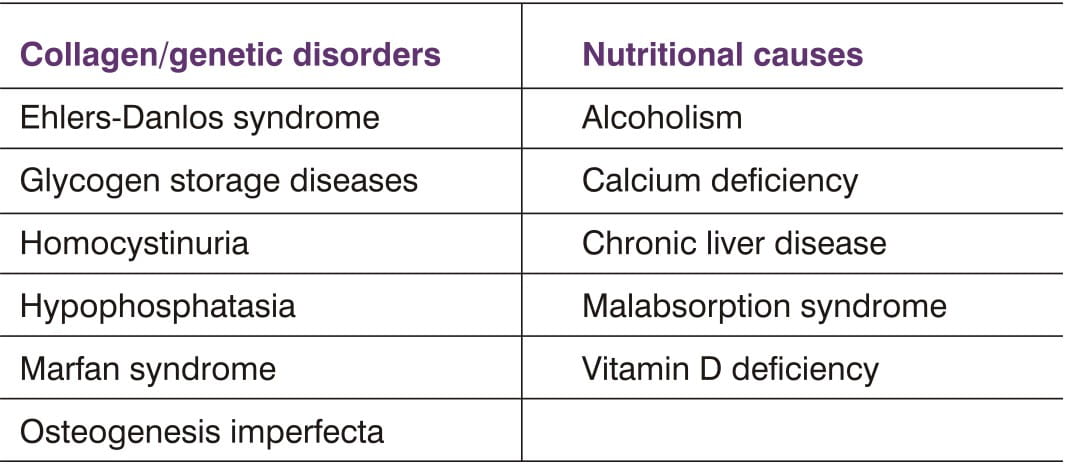
Adapted from Tresolini CP, Gold DT, Lee LS, eds. Working with patients to prevent, treat and manage osteoporosis: a curriculum guide for health professionals. 2nd ed. San Francisco National Fund for Medical Education, 1998
Glucocorticoid therapy is the most frequent cause of drug-induced osteoporosis. Skeletal effects of glucocorticoids are dose-dependent, with doses of prednisolone at or above 5 mg/day resulting in significant bone loss and increased fracture risk. Bone loss occurs even with low-dose glucocorticoid therapy. No threshold dose, below which bone loss does not occur, has been identified.
Loss of bone mass is most rapid during the first year of glucocorticoid therapy and significant reductions can be seen as soon as 3 months after starting therapy. Even relatively short courses of oral glucocorticoids can produce rapid bone loss. Use of topical as opposed to oral glucocorticoids reduces medication-related adverse effects.
As bone loss ensues, fracture risk increases. Decreased BMD and subsequent fractures are seen predominantly in areas rich in trabecular bone, such as the vertebrae and ribs.
Thus, glucocorticoid-induced osteoporosis contributes to a significant increase in morbidity for individuals who already may have substantial disability as a result of their primary disease.
The cardinal feature of glucocorticoid-induced osteoporosis is decreased bone formation, evidenced by decreased wall thickness of bony trabeculae and decreased work output by osteoblasts. Glucocorticoids accelerate bone loss in several ways, although the exact mechanisms of the effects of glucocorticoids on bone and calcium metabolism have not been fully elucidated. Proposed mechanisms include increased bone resorption, decreased osteoblast proliferation and biosynthetic activity, sex-steroid deficiency (via direct effects on the gonads and inhibition of pituitary gonadotropin secretion), and secondary hyperparathyroidism (from decreased intestinal calcium absorption and hypercalciuria due to defective vitamin D metabolism).
See section "Making The Diagnosis Of Osteoporosis".
Preventive measures
Because bone loss is greatest during the initial months of therapy, preventive measures should be started at the beginning of glucocorticoid therapy. Glucocorticoids should be used in the lowest effective dose possible. Lifestyle modifications to reduce bone loss should be encouraged. The American College of Rheumatology recommends that all persons taking glucocorticoids receive 1,500 mg/day of calcium through diet or supplements plus 800 lU/day of vitamin D or 0.5 μg/day of calcitriol.
Bisphosphonates have been shown to be highly effective in primary and secondary prevention of glucocorticoid-induced osteoporosis in men and women. Risedronate is approved by the US FDA for both prevention and treatment of glucocorticoid-induced osteoporosis, and alendronate is approved for treatment. Calcitonin also prevents corticosteroid-induced bone loss. There are limited data to support the use of HRT to treat osteoporosis in patients receiving prolonged therapy with glucocorticoids.
Osteoporosis is often called the "silent disease" because bone loss generally occurs without symptoms. Height loss, spinal deformity and fragility were once considered inevitable consequences of growing old. These features are now recognized as symptoms of osteoporosis.
Osteoporosis may not be diagnosed until the bones become so weak that a sudden strain, bump, or fall causes a hip fracture or a vertebra to collapse. Collapsed vertebra may initially be felt or seen in the form of severe back pain, loss of height, or spinal deformities such as kyphosis, or severely stooped posture.
History and physical examination are neither sensitive enough nor sufficient for diagnosing primary osteoporosis. However, they are important in screening for secondary forms of osteoporosis and directing the evaluation.
Possibility of osteoporosis and fracture risk should be considered in all postmenopausal women, based on the presence of the risk factors. Bone mineral density measurement is the most important technique to establish the diagnosis of osteoporosis.
Clinical, biochemical, routine radiological, CT scan and bone biopsy are also useful in diagnosing osteoporosis.
BMD is the most important determinant of bone strength. It is currently the best predictor available for fracture risk. BMD has a continuous, graded, inverse relationship to the risk of fracture: the lower the BMD, the greater the fracture risks.
BMD can be Used To
- Detect low bone density before a fracture occurs.
- Confirm a diagnosis of osteoporosis if one already had a fracture.
- Determine the rate of bone loss and/or monitor the effects of treatment if the test is conducted at intervals of a year or more.
Measurements of BMD at any skeletal site have value in predicting fracture risk. A variety of densitometers are in clinical use and provide reliable assessment of fracture risk. BMD is measured in the spine, wrist, hip, heel or hand. However, hip BMD is the best predictor of hip fractures, and it predicts fractures at other skeletal sites also. BMD is expressed as a relationship of two norms: the expected BMD for the patient's age and sex (Z-score), or for "young normal" adults of the same sex (T-score). The difference between the patient's score and the norm is expressed in standard deviations (SD) above or below the mean (usually, 1 SD equals 10-20% of the bone density value). T-scores decline in parallel with the steady drop in bone mass that occurs with aging. The Z-score may be helpful in diagnosing secondary causes of bone loss.
The World Health Organization (WHO) has established the following definitions based on bone mass measurement at the spine, hip, or wrist in postmenopausal women:
- Normal: BMD is within 1 SD of a "young normal" adult (T-score at -1.0 and above).
- Low bone mass (osteopenia): BMD is between 1 and 2.5 SD below that of a "young normal" adult (T-score between -1 and -2.5).
- Osteoporosis: BMD is 2.5 SD or more below that of a "young normal" adult (T-score at or below -2.5). Women in this group who have already experienced one or more fractures are deemed to have severe or "established" osteoporosis.
Although these definitions are necessary to establish the prevalence of osteoporosis, they should not be used as the sole determinant of treatment decisions.
Indications for BMD Measurements
There is insufficient evidence for routine screening of osteoporosis. The decision to test for BMD should be based on an individual's risk profile, and testing is never indicated unless the results could influence a treatment decision.
BMD Testing Should be Performed On
- All women aged 65 and older regardless of risk factors.
- Younger postmenopausal women (<65 years) with one or more risk factor (other than being white, postmenopausal, and female).
- Postmenopausal women who present with fractures (to confirm diagnosis and determine disease severity).
BMD Testing Techniques
All of the tests described below are good predictors of future fracture risk.
1. Dual Energy X-ray Absorptiometry (DEXA, DXA, rarely also called QDR, DPX, DER): Today DEXA is the most completely developed, reliable, and popular method in use for measuring BMD. It is considered as the "gold standard". DEXA was developed in the 1980s and its widespread use began in 1988. The skeletal site is exposed to two X-ray beams of different intensity, and the mineral content of the bone is calculated by means of computer programs from the amount of radiation absorbed. Using the results of the two measurements, the effects of the soft tissue components (different quantities of muscle and fatty tissue) can be calculated and discarded. DEXA can measure central (hip and spine) and peripheral (forearm) sites, and can even perform a total body scan ("full body DEXA scanner").
The hip joint and the lumbar spine are routinely measured from the front (Anterior Posterior) or the side (lateral). The combined evaluation of these two measurements improves the assessment of a patient's bone mineral status and the fracture prediction, especially in cases with anatomic variations, severe degenerative changes, or fractures. The measurements of the lumbar spine are not confined to the vertebral bodies; they also include the arches and spinous processes, which have a considerable quantity of compact bone.
Two terms, T-score and Z-score, are commonly used to report DEXA results and both of these rely on a standard deviation (SD) for the measurement. SD represents the normal variability of a measurement in a population; the difference between the 5th and 95th percentile of a group covers about 4 SDs. One SD of the hip or spine BMD corresponds to about 10-15% of the mean value.
- Z-score is the number of SDs below (minus) or above (plus) the mean BMD value for people of the same age ("age and sex matched" controls).
- T-score is the number of SDs below or above the mean value of BMD for young (20-30-year old) adults ("peak bone density").
Because BMD declines with age at all sites, after age 30, the T-scores are lower than the Z-scores, and the differences increase with age. By definition, diagnosis of osteoporosis is based on a T-score of < -2.5 SD.
The International Society of Clinical Densitometry (ISCD) suggests measurement of at least two sites, if possible, and recommends that diagnosis be based on the lowest T-score. It suggests using the L2-L4 average, measurement rather than a single vertebra, if possible. In measurements hip, either the total hip or the femoral neck measurement is used, whichever is the lowest standard deviation.
DEXA is available at specialised centres and costs between Rs. 1,500 - 2,000. The important advantages of DEXA are:
- It is not invasive; the patient remains clothed and it is, therefore, not a burden to the patient.
- It is very quickly carried out (5-10 min).
- It is cost-effective.
- It has a very low radiation dose (1-3 mRem equivalent to 1/10-1/100 of a normal X-ray film).
- It measures those skeletal areas most vulnerable to osteoporosis and to fractures - the lumbar spine and the hips.
- The measurements are accurate and therefore, ideal for follow-up and control investigations (accuracy error 1-10%, precision 1%).
- It is recognized by the WHO as the standard method for definition of diagnosis.
2. Peripheral Dual X-ray Absorptiometry (pDEXA): This is DXA at peripheral sites like forearm, finger or heel.
3. Single-energy X-ray Absorptiometry (SXA): SXA uses a single-energy X- ray beam for measurement. This method is still used today to measure the bones of the ankle because of the paucity of surrounding soft tissue.
4. Quantitative Computed Tomography (QCT): QCT measures trabecular and cortical bone density at several skeletal sites, but is most commonly used to measure trabecular bone density in the spine. It provides three dimensional volumetric measurements reported in mg/cc. It uses a conventional CT scanner with a calibration phantom. It is also possible to measure trabecular and cortical bone density in the periphery by pQCT.
5. Quantitative Ultrasound (QUS): Ultrasound assesses bone in the heel, tibia, patella, or other peripheral sites where the bones are relatively superficial. Ultrasound measurements are generally not as precise as DEXA or SXA, but appear to predict fracture risk as well as other measures of bone density.
6. Other tests
Laboratory tests: Basic chemical analysis of serum and urine is indicated when the history suggests other clinical conditions influencing the bone density. These tests provide specific clues to serious illnesses that may otherwise have gone undetected and which, if treated, could result in resolution or modification of the bone loss.
Routine radiology: Shows the reduction of width of the cortex with thinning of trabeculae. There may be wedging and fracture of vertebrae, yet pedicles may be intact. Unless more than 30% bone mass is lost, conventional X-rays do not show osteoporosis.
Computerised Tomography (CT) Scan: Routine CT scans helps to exclude tuberculosis, secondary deposits and multiple myeloma. Purpose built isotopic quantitative CT devices measure trabecular bone separate from cortical bone mass. They are costly and entail radiation hazards.
Needle Bone Biopsy: Differentiates osteoporosis from osteomalacia and carcinoma. Bone marrow examination may be needed to exclude myeloma or secondaries.
Metabolic bone diseases other than osteoporosis, such as hyperparathyroidism or osteomalacia, may be associated with a low BMD. Many of these diseases have very specific therapies and it is appropriate to complete a history and physical examination before attaching a diagnosis of osteoporosis on the basis of a low BMD alone. In patients in whom a specific secondary, treatable cause of osteoporosis is being considered, relevant blood and urine studies (such as urine calcium, thyrotropin, protein electrophoresis, Cortisol or antibodies associated with gluten-sensitive enteropathy) should be obtained prior to initiating therapy.
For instance, elderly patients with recent fractures should be evaluated for osteomalacia with a 25-hydroxyvitamin D level. Limited biochemical testing (such as serum calcium, creatinine, etc.) may be appropriate for anyone with osteoporosis. Osteoporosis and osteoarthritis are two different medical conditions with little in common. However, people with rheumatoid arthritis may be more likely to develop osteoporosis, especially as a secondary condition from the medications used to treat it.
The US Preventive Services Task Force (USPSTF), the National Osteoporosis Foundation (NOF), the American Association of Clinical Endocrinologists (AACE) and the American College of Obstetricians and Gynaecologists (ACOG) have recommended that:
- Bone mineral density testing should be done in all postmenopausal women who are 65 years of age or older.
- Bone mineral density testing should be done in all postmenopausal women younger than 65 years of age who have one or more risk factors (e.g. family history, glucocorticoid therapy, sedentary lifestyle, etc.) for osteoporosis.
- Bone mineral density testing should be performed on all postmenopausal women who have fractures to confirm the diagnosis of osteoporosis and determine disease severity.
- In the absence of new risk factors, screening should not be performed more frequently than every two years.
- Women should be counselled on the risk of osteoporosis and related fragility fractures. Such counselling should be a part of the annual gynaecologic examination.
Today in the new millennium, it is completely unacceptable that half of all postmenopausal women should suffer fractures when these can be avoided by adequate preventive measures. Therefore, women should be counselled about the following preventive measures:
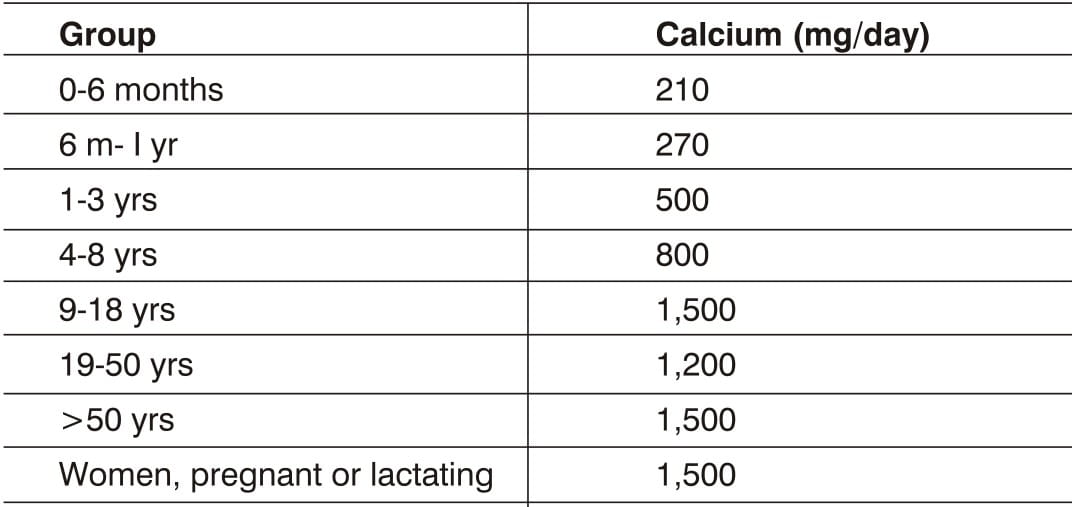
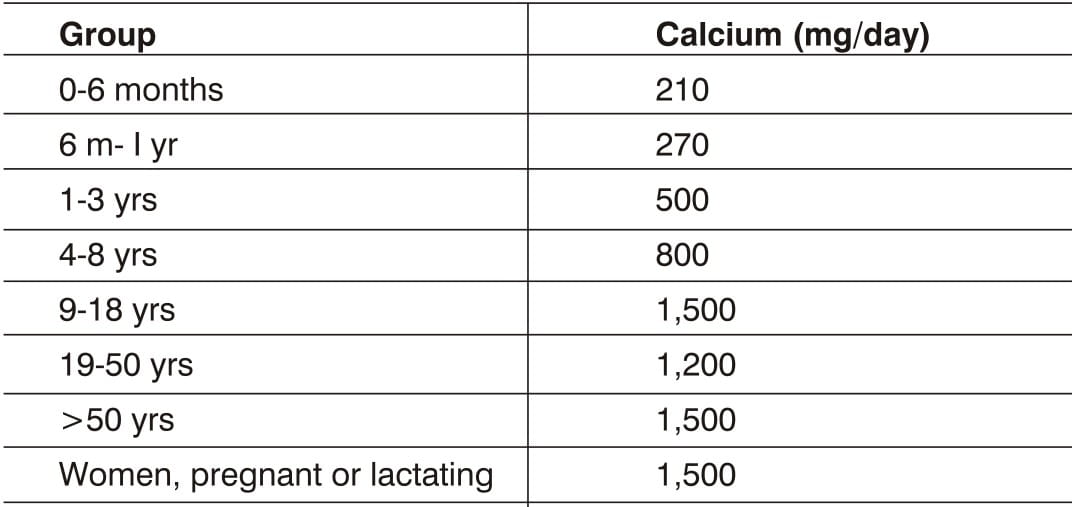
- Adequate calcium consumption (see Table 3), and using dietary supplements if dietary sources are not adequate.
- Adequate vitamin D consumption (400 to 800 IU daily), preferably from the natural sources of this nutrient.
- Regular weight-bearing and muscle-strengthening exercise to reduce falls and prevent fractures.
- Smoking cessation.
- Moderation of alcohol intake.
- Fall-prevention strategies.
- Pharmacotherapy.
The goal of management of osteoporosis is to prevent fractures. This can be accomplished by:
- Achieving the highest possible peak bone mass
- Preventing further bone loss, and
- Minimising chances for injury.
These objectives can be addressed through lifestyle modifications and pharmacologic therapy.
An adequate intake of calcium, lifelong, is necessary for the acquisition of peak bone mass and maintenance of bone health. The skeleton contains 99% of the body's calcium stores; when the exogenous supply is inadequate, bone tissue is reabsorbed from the skeleton to maintain serum calcium at a constant level.
Vitamin D promotes bone formation by improving intestinal absorption of calcium and phosphate and by stimulating maturation and mineralisation of the osseous ground substance - the osteoid. A daily allowance of 400-800 IU is required for healthy bone.
The effects of calcium and vitamin D supplements on bone are not as dramatic as those achieved with pharmacological agents. Nevertheless, adequate calcium and vitamin D intake is considered essential for prevention and treatment of osteoporosis.
Sedentary lifestyle is associated with rapid reduction in BMD. Regular weight-bearing and muscle-strengthening exercises reduce the risk of falls and fractures and appear to be a highly effective preventive measure for osteoporosis.
Among its many health benefits, weight-bearing and muscle-strengthening exercises can improve agility, strength, and balance, which may reduce the risk of falls. In addition, exercise may increase bone density modestly. The National Osteoporosis Foundation (NOF) strongly endorses lifelong physical activity at all ages, both for osteoporosis prevention and overall health, as benefits are lost when the person stops exercising.
Patients should be advised to avoid tobacco smoking and reduce alcohol intake. The use of tobacco products is detrimental to the skeleton as well as to overall health.
In addition to exercises, strategies to reduce risk of falling include, but are not limited to, checking and correcting vision and hearing, evaluating any neurological problems, reviewing prescription medications for side effects that may affect balance and stability, and providing a check list for improving safety at home. Wearing undergarments with hip protectors may protect an individual from injuring the hip in the event of a fall. Hip protectors should be considered for patients who have significant risk factors for falling or who have previously fractured a hip.
All patients being considered for drug treatment of osteoporosis should also be counselled on risk factor reduction. Patients should be counselled specifically on the importance of calcium, vitamin D, and exercise as part of any treatment programme for osteoporosis. Prior to initiating treatment, patients should be evaluated for secondary causes of osteoporosis and have central DEXA measurements, when available. Pharmacological agents for osteoporosis alter the balance of bone remodelling by increasing bone formation or reducing bone resorption.
Pharmacotherapy should be initiated in:
- Postmenopausal women who experienced a fragility or low-impact fracture.
- A person with BMD T-scores below -2.0 by hipDEXA with no risk factors.
- A person with BMD T-scores below -1.5 by hip DEXA with one or more risk factors.
- Bisphosphonates [Alendronate, Risedronate]
- Estrogens (estrogen and/or hormone therapy)
- Calcitonin
- Parathyroid hormone
- Selective estrogen receptor modulators [Raloxifene ]
- Strontium Ranelate
- Others: Calcitrol, Tibolone, Sodium fluoride
Bisphosphonates are a class of drugs that reduce bone loss, increase bone density in both the spine and hip, and reduce the risk of spine and hip fractures by directly inhibiting resorption and hindering recruitment and activity of the osteoclasts at the surface of the bone. Previously, HRT was widely recommended as a means of prevention for osteoporosis; however, many women are now opting for bisphosphonates because these medications are not associated with the same increased risks noted with use of HRT and they appear more effective than HRT. Alendronate and Risedronate are examples of drugs in this category.
Alendronate : Alendronate was the first bisphosphonate (1995) to be approved by the US FDA for treatment of osteoporosis. It is a nitrogen-containing bisphosphonate, which binds to bone surfaces, and inhibits bone resorption by osteoclasts, possibly through inhibition of the mevalonate pathway. Oral alendronate produces sustained increases in BMD. It is effective and well tolerated in the:
- Treatment of women with primary (including postmenopausal) osteoporosis.
- Treatment of men with primary osteoporosis.
- Treatment of corticosteroid-induced osteoporosis.
- Prevention of osteoporosis in postmenopausal women.
Controlled clinical trials of 5 years' duration in patients with osteoporosis or low BMD treated with alendronate demonstrate that it increases bone density by 5-10% at the spine and hip, and decreases the risk of fracture at these sites by about 50%. Bone loss resumes once a patient stops taking alendronate, but this is not accelerated as compared with placebo. Thus, previous gains in BMD are maintained, but continued therapy is required to obtain progressive increases in BMD.
The dose of alendronate for prevention and treatment of postmenopausal osteoporosis is 5 mg/day and 10 mg/day respectively. The US FDA recently approved once-weekly dosing of alendronate; 35 mg once weekly for prevention of bone loss and 70 mg once weekly for treatment of postmenopausal osteoporosis.
Risedronate Risedronate (approved by the US FDA in 2000) is a novel, orally administered pyridinyl bisphosphonate indicated for:
- Prevention of postmenopausal osteoporosis
- Treatment of postmenopausal osteoporosis
- Prevention of glucocorticoid-induced osteoporosis
- Treatment of glucocorticoid-induced osteoporosis
The drug reduces bone turnover and decreases resorption chiefly through osteoclastic effects, with no undesirable effects on cortical porosity or thickness or on cancellous bone volume. Risedronate prevents bone loss in postmenopausal women and in patients taking glucocorticoids. Bone loss prevention study in women with recent menopause (within 6 months to 3 years) showed statistically significant increases, relative to both baseline and placebo, with risedronate 5 mg/day in spinal and hip BMD from as early as 3 months after starting treatment.
Risedronate increases BMD in patients with osteoporosis. Double-blind trials have shown that vertebral fracture incidence was reduced by risedronate 5 mg/day by up to 65% and 49% relative to placebo after 1 and 3 years, respectively. Risedronate improved lumbar spine, femoral neck and femoral trochanter BMD in a statistically significant rate relative to placebo. The drug is a valuable option with first-line potential, particularly in patients for whom hormonal therapy is inappropriate. The effects of the drug on hip fracture incidence in elderly women with confirmed osteoporosis point to a particular role in older patients, or those with more advanced disease.
Estrogen/hormone therapy (HT) is approved by the US FDA for the prevention of osteoporosis, relief of vasomotor symptoms and vulvovaginal atrophy associated with menopause. However, the FDA recommends that when HT use is considered solely for prevention of osteoporosis, approved non-estrogen treatments should first be carefully considered. Because of the risks, HT should be used in the lowest possible doses for the shortest duration to meet treatment goals.
Calcitonin inhibits bone resorption by blocking osteoclastic activity. There is evidence that markers of bone turnover decrease, and that bone mineral density stabilizes (or even increases) with use of calcitonin. It is approved for the treatment of osteoporosis in women who are at least 5 years postmenopausal. Calcitonin can be given by nasal inhalation or subcutaneous or intramuscular injection.
The physiological function of parathyroid hormone is to maintain extracellular calcium levels. It acts either directly on target cells or indirectly through the synthesis of 1, 25-dihydroxyvitamin D. Evidence suggests that parathyroid hormone has a dual action on bone, with both osteoblasts and osteoclasts being responsive to this hormone. The resorptive effect predominates when levels of parathyroid hormone are elevated continuously, but an anabolic effect on bone is seen with interrupted dosing. Parathyroid hormone has been approved by the FDA for the treatment of osteoporosis in postmenopausal women at high risk of fracture. It is generally well tolerated, but patients need to be closely monitored because of the risk of hypercalcaemia. The safety and efficacy of parathyroid hormone has not been demonstrated beyond 2 years of treatment and it is very expensive. The studies showed that the risk of vertebral fracture was reduced by 70% within 18 months of treatment and the nonvertebral fracture risk was reduced by 50%. Injectable PTH is available in India but the high cost of the product is something people find an inhibiting factor. The therapy lasts for 18 months to 24 months and the osteoblastic action is evident. In our country there is a general consensus among the experts owing the exorbitant cost of treatment that PTH therapy shall be reserved for patients who do not show improvement despite other treatments or sustain fracture while being on antiresorptive therapy.
The selective estrogen receptor modulator, raloxifene, has been approved by the FDA for both prevention and treatment of osteoporosis in postmenopausal women. It functions as either an antagonist or an agonist at specific estrogen receptors.
Raloxifene stimulates bone while blocking the effects of estrogen in the breast and uterus. Although it is a good choice of therapy for women with a history of breast or uterine cancer or for women with concerns about taking estrogen, it tends to induce vasomotor symptoms. Other side effects of leg cramps and venous thrombo embolic events have been reported. It may also be a better choice of therapy for women with severe gastrointestinal symptoms and for those who have difficulty tolerating the bisphosphonates. This class of drugs should be used with extreme caution for women who are perimenopausal because the drug is contraindicated in pregnancy.
Strontium ranelate is a new, effective and safe treatment for vertebral and hip osteoporosis, with a unique mode of action, increasing bone formation and decreasing bone resorption, leading to a rebalance of bone turnover in favour of bone formation. Strontium ranelate increases collagen and non-collagen protein synthesis by mature osteoblast-enriched cells. It dose-dependently inhibits preosteoclast differentiation.
Calcitrol: This synthetic vitamin D analogue, which promotes calcium absorption, has been approved by the US FDA for managing hypocalcaemia and metabolic bone disease in renal dialysis patients. However, no reliable data demonstrate a reduction of risk for osteoporotic fracture.
Tibolone: Tibolone is a tissue-specific, estrogen-like agent that may prevent bone loss and reduce menopausal symptoms, but it does not stimulate breast or uterine tissue.
Sodium Fluoride: Through a process that is still unclear, sodium fluoride stimulates the formation of new bone. The quality of bone mass thus developed is also uncertain, and the evidence that fluoride reduces fracture risk is conflicting and controversial.
Combination Therapy: A bisphosphonate with a non-bisphosphonate can provide additional small increases in BMD when compared with monotherapy; however, the impact of combination therapy on fracture rates is unknown. The added cost and potential side effects should be weighed against potential gains.
Once patients have been identified and treatment initiated, it is important to arrange adequate follow-up to reinforce the importance of compliance with treatment and to evaluate the response. At minimum, all treated patients should be seen after 3 to 6 months of treatment and thereafter, at least annually.
The response to therapy can be monitored using tests of biochemical markers such as N-terminal or C-terminal crosslinks of type 1 collagen, serum osteocalcin, or serum bone-specific alkaline phosphatase. Repeat BMD measurement may be of value in assessing compliance and providing patient feedback. However, changes in BMD occur over a longer period, and it is generally not useful to repeat BMD measurement until completion of 1 or 2 years of therapy and every 2 years thereafter. The majority of patients receiving efficacious therapy will have a measurable increase in BMD at the spine and hip (especially at the trochanter subregion) after 2 years of treatment).
Osteoporosis was regarded as a "woman's disease", but it is now clear that the problem of osteoporosis occurs in men also. Men with osteoporosis account for approximately one-fifth of all patients with osteoporosis. It develops less often in men than in women because men have more bone mass; bone loss starts later and progresses more slowly, and there is no period of rapid hormonal change and accompanying rapid bone loss.
The amount of tissue or bone mass in the skeleton reaches its maximum amount by the late twenties. By this age, men accumulate more bone mass than women. After this point, the amount of bone in the skeleton typically begins to decline slowly as removal of old bone exceeds formation of new bone.
In their fifties, men do not experience the rapid loss of bone mass that women have in the years following menopause. By age 65 or 70 years, however, men and women lose bone mass at the same rate, and the absorption of calcium, an essential nutrient for bone health throughout life, decreases in both sexes. It is well known that loss of estrogen causes osteoporosis in women. Recent research suggests that estrogen deficiency such as in hypogonadism may be a cause of osteoporosis in men also.
It is estimated that up to 30 % of men with osteoporotic vertebral fractures have low testosterone levels. Testosterone levels decrease gradually with age, but medications like steroids, cancer treatments (especially for prostate cancer), and many other factors can affect testosterone levels.
Testosterone replacement therapy may be helpful in preventing or slowing bone loss. Its success depends on factors such as age and the duration of time for which testosterone levels have been reduced. Also, it is not yet clear how long any beneficial effect of testosterone replacement will last; therefore, osteoporosis is usually treated directly, using medications approved for this purpose.
Though osteoporosis rarely occurs in children, it may cause severe pain, multiple fractures, and life-long limitations of movement and locomotion when it does occur. Osteoporosis in children is often not diagnosed until after one or two fractures have occurred, or if low density is suspected on X-rays.
Osteoporosis in children has not yet been officially defined. The WHO definition is based on values for adults. In practice, however, the diagnosis is also based on a bone density measurement. More than 2 SD below the average value of a child of similar age with healthy bones is considered as osteoporosis.
Treatment of childhood osteoporosis includes general measures such as:
- Adequate pain relief in children with vertebral fractures.
- Orthopaedic procedures to fix fractures of the long bones.
- Physiotherapy with rehabilitation to improve muscle strength.
- Periods of bed rest in paediatric illness should be minimized.
Literature on the medical treatment of childhood osteoporosis is limited and still not evidence-based, but some studies have reported that calcium, vitamin D, calcitriol and calcitonin are useful.
It is important to realize that spontaneous improvement without any medical treatment may occur. Thus, in some children with osteoporosis, it may be appropriate to monitor their progress over time and "watch and wait". This would also depend on the cause of osteoporosis.
Osteoporosis poses a major public threat and arresting this disorder should be the primary goal of our preventive efforts in the coming years.
Although it primarily affects postmenopausal women, individuals of any age or gender can be affected. Multiple lifestyle factors can increase the risk for acquiring the disease. Osteoporosis is a multifactorial condition and its prevention and treatment must involve all possible options - from rather simple fall-preventive measures to the use of pharmacological agents.
Individualised therapy is the key to prevention and treatment of osteoporosis. Evidence demonstrates the efficacious use of calcium and vitamin D supplementation, bisphosphonates, HRT, raloxifene, and calcitonin for stabilization and improvement in BMD. Drugs may decrease a patient's risk of fracture even when there is no apparent increase in BMD. Repeat bone density measurements for monitoring disease progression in response to therapy should generally be performed after 1 or 2 years.
Osteoporosis needs lifelong management and adherence to therapy is a must to gain benefit and reduce risk of fractures.
Increasing knowledge of the mechanisms that regulate bone cell activity will provide sources for potential new therapeutic strategies. Thus, future approaches may include local regulators, such as cytokines (which are essential in bone metabolism), modification of hormone receptors, and pharmacogenetics.
With the advent of newer effective therapies for prevention and treatment of osteoporosis, height loss, spinal deformity and increased bone fragility that were once regarded as an inevitable consequence of growing old are no longer considered so.
1. American Family Physician 2001; 63(5): 897-904
2. American Family Physician 2004; 69(6): 1-4
3. Am J Health-Syst Pharm 2004; 61(17): 1801-1811
4. BioMed 2001; 27-30
5. Bulletin of the World Health Organisation 2003; 81 (9): 657-664
6. Clinical Therapeutics 1999; 21 (6): 1025-1044
7. Drugs 2001; 61(5): 655-712
8. Drugs 2001; 61(7): 999-1039
9. http://www.cor.uams.edu/summary_of_bmd.htm. Last accessed on 22-07-05
10. J Midwifery Womens Health 2003; 48(1): 39-54
11. Obstetrical and Gynaecological survey 2001; 56(8): 492-504
12. Obstetrical and Gynaecological survey 2000; 55 (12): S49-S55
13. Osteoporos Int 2003; 14: 2-12
14. Osteoporosis-Diagnosis, Prevention, Therapy. Berlin Heidelberg: Springer-Verlag; 2004
15. Postgraduate Medicine 2000; 107 (7): 37-56
16. Postgraduate Medicine 2002; 78: 526-532
17. Preventive Medicine 2003; 36: 243-249
18. The Annals of Pharmacotherapy 2003; 37: 711 -724
19. The Medicine Group (Journals) Ltd 1997; 76-83
20. The New England Journal of Medicine 2004; 350 (5): 504-506
21. The New England Journal of Medicine 2005; 353(2): 164-171